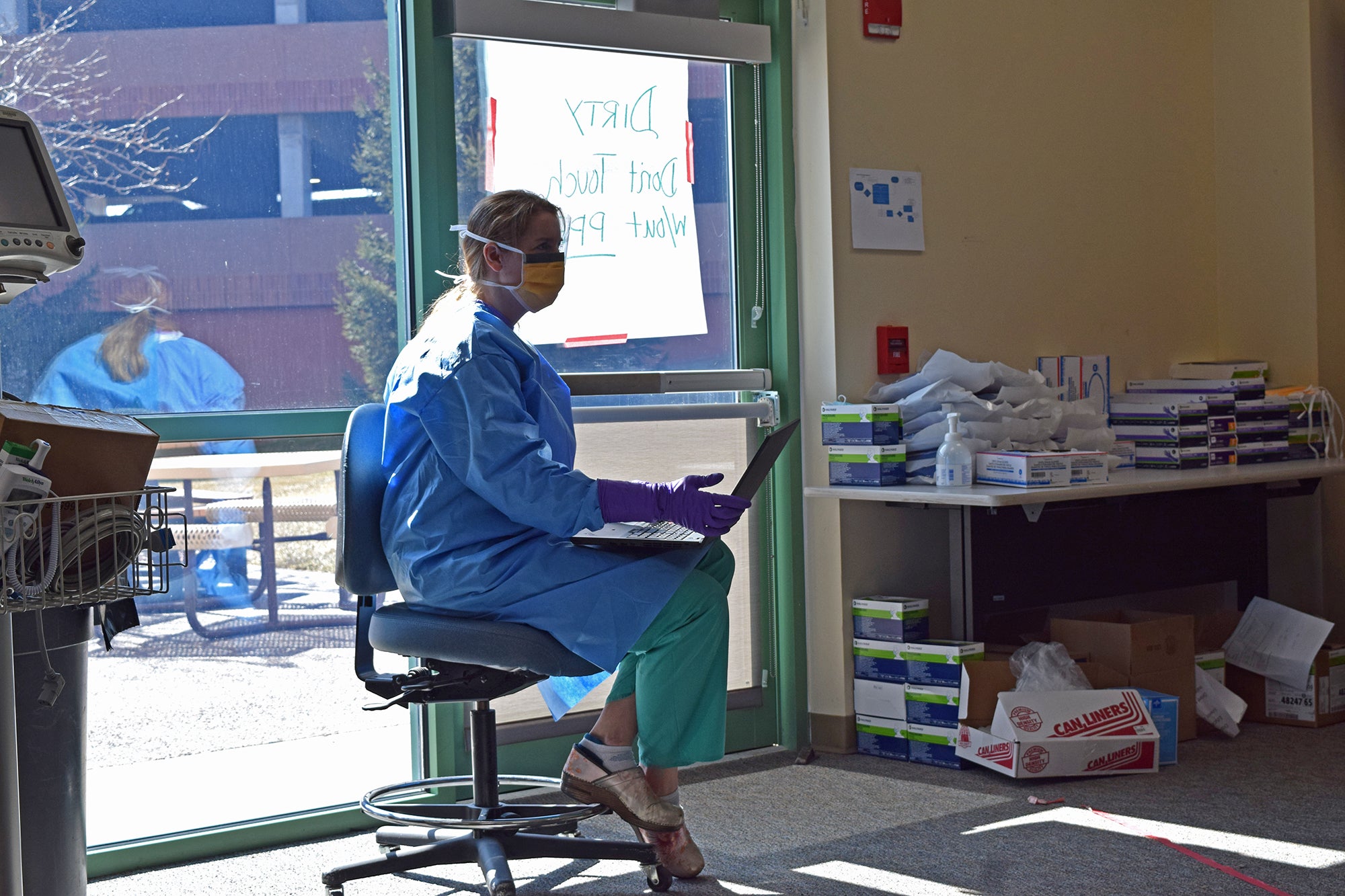
Hospitals and clinics are changing practices as they respond to the new coronavirus pandemic. Medical facilities across Wisconsin are postponing routine appointments or elective procedures. The rapidly evolving medical landscape is leaving physicians with tough decisions on who to treat in person and who to turn away.
Some are following the recommendation of the Centers for Disease Control and Prevention (CDC), Surgeon General and American College of Surgeons to postpone elective procedures, including Froedtert Health, Aurora Health Care, Children’s Wisconsin and Marshfield Clinic Health System, SSM Health, UW Health, UnityPoint Health-Meriter, Mayo Clinic, and Essentia Health in Duluth. Many facilities are asking people to call their doctor before seeking care at a hospital or clinic.
Dr. Anthony Sturm is a family medicine physician at Wildwood Family Clinic in Madison. He said they’ve been doing their best to follow recommendations from the CDC, as well as state and local public health officials.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
Sturm said his main focus is the health of the patient and anyone that person may come in contact with during a visit.
“There are patients who are sick enough and high enough risk, they need to go to a place that has capacity if they need to be hospitalized,” Strum said. “If a patient is not very sick, but is at higher risk, we’re, at this point, we’re telling them to stay home. Whereas earlier this week, we’re telling them to come in to get swabbed.”
If he were able, Sturm said he would test every patient exhibiting symptoms, but his office has fewer than 20 tests at the moment. Sturm said he and his staff are doing their best to keep up on the latest developments and provide the best guidance on whether to seek treatment or testing.
“It’s been really hard on patients. It’s been really hard on staff, and hard on us just trying to figure out what to do,” he said. “But, generally under most circumstances if somebody seems like they could be infectious, we’re telling them to just not come into clinic because there’s not necessarily a lot we’re going to be able to do for them.”
Sturm said they’re still providing supportive care and conducting visits through telemedicine or by video conferencing to limit contact.
Dr. Jeffrey Pothof, chief quality officer for UW Health in Madison, said they’ve been telling providers to determine which appointments are urgent, such as procedures that were time-sensitive or could extend a patient’s life. Doctors have been reaching out to patients to communicate whether they’re rescheduling appointments and the reasons. For the most part, he said they’ve received a positive response.
As changes arise, Pothof said their incident command team is doing their best to communicate that to patients and staff.
“I think at this point, everyone realizes that this is changing so rapidly,” he said, noting they’ve been sending out emails about new developments. “We’ve been pretty quickly able to get our doctors and our nurses and other staff kind of up to speed on like this screening for tests that just changed.”
Now, UW Health is prioritizing tests for health care workers and individuals who are at high risk for contracting the new coronavirus after the State Lab of Hygiene informed them they were overwhelmed with tests.
Dr. Brad Wozney, a family care physician at Bellin Health Denmark, said his office is receiving a lot of requests for testing.
“We are getting a lot of patients who are calling us asking to be tested to prove that they don’t have the virus, and that is absolutely not going to happen,” he said. “We don’t have enough test kits or the ability to just test people without symptoms.”
Wozney said they’re also trying to triage patients by phone and reaching out to them on the status of their upcoming appointments.
Dr. Bridget Pfaff at Gundersen Health System in La Crosse said they don’t want people to call in with questions about their upcoming medical visits or procedures.
“We will be contacting you,” she said. “We want you to call us if you have signs and symptoms of infection, and you think you might need to be tested for this infection.”
Jason Akl, chief operations officer for NorthLakes Community Clinic, said they’re doing as much as possible to keep appointments with individuals at their medical clinics in northern Wisconsin. Dental practices will now only include emergency procedures.
He said their clinics are removing potential exposures by utilizing resources at area hospitals or offering curbside testing at three clinic locations in Iron River, Minong and Lakewood. The federally qualified health center is hoping to provide telehealth services as well.
“We’re waiting for Medicaid to come out with the guidelines. You know, we are all set up to do telehealth services, but we need the go ahead from the Medicaid office,” said Akl. “We’re excited to offer potential services for our patients through medical or behavioral health to help, but right now we just don’t have regulations to do that.”
In the meantime, he said they’re asking individuals who are at high-risk for the disease not to come into the clinic. They’re also taking steps to triage individuals and requiring people to wear a mask if they’re experiencing symptoms.
On Wednesday, Children’s Wisconsin said 200 patients and health care workers at its hospital are being tested for coronavirus after a doctor treating at-risk kids tested positive for the disease.
Editor’s note: This story will be updated. Danielle Kaeding, Hope Kirwan and Megan Hart contributed reporting for this story.
Wisconsin Public Radio, © Copyright 2026, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.