This story was produced and republished by Wisconsin Watch and WPR.
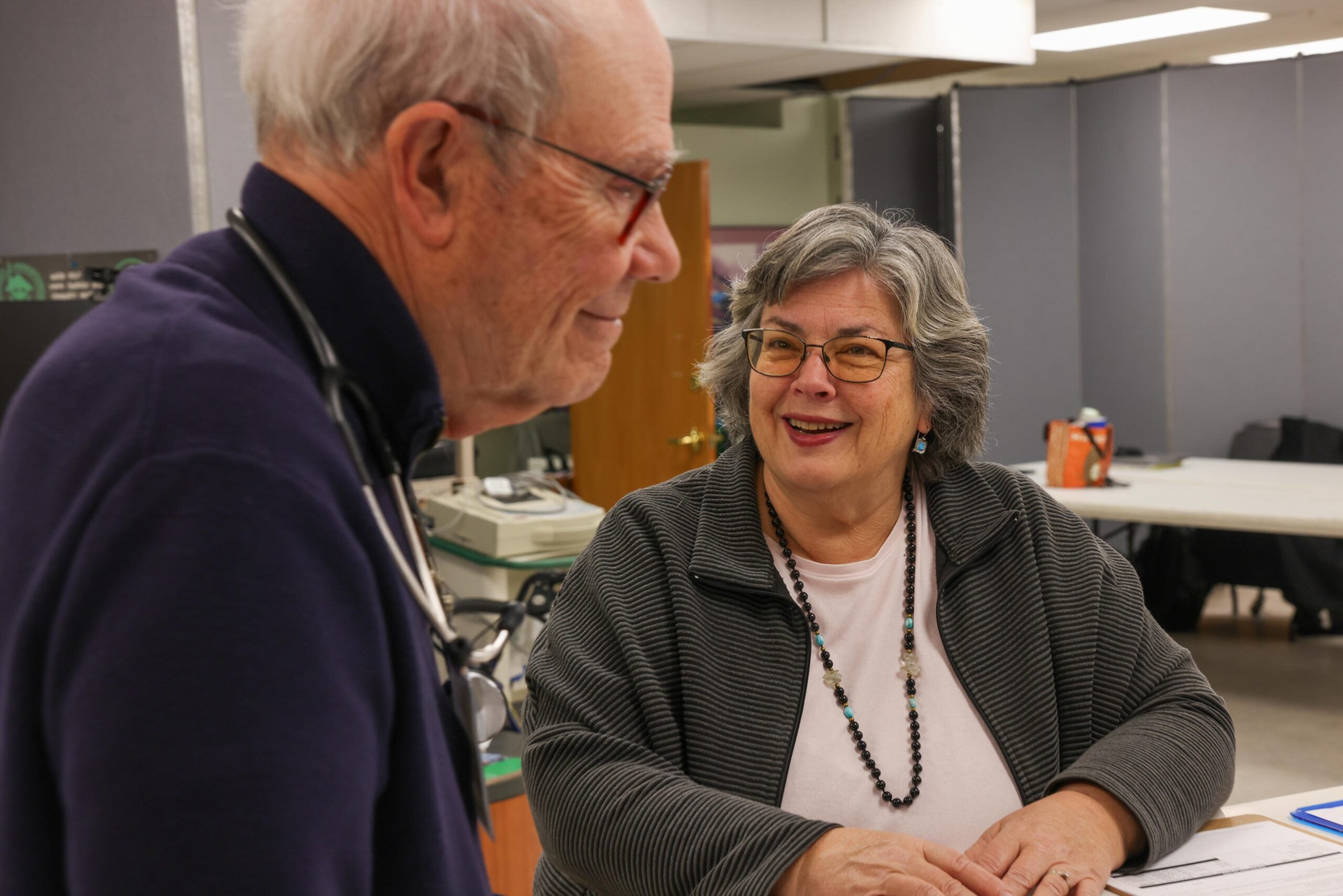
Cars filled the small parking lot outside of Milwaukee’s Cross Lutheran Church on a recent Monday afternoon. The church’s pews sat empty, but downstairs visitors waited around folding tables. Not to hear a sermon, but to see a volunteer physician.
Staff and volunteers walked patients past a row of dividers used to separate the “waiting room” from the folding tables where doctors and counselors filled out paperwork.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
In front of the free health clinic’s four exam rooms, two phones rang.
“This is the Bread of Healing Clinic. Can you hold for a moment?” asked Diane Hill Horton, the free health clinic’s assistant.
Across from Hill Horton, another staff member scheduled an appointment in Spanish.
On a typical Monday, the clinic sees up to 30 patients. Bread of Healing treated 2,400 patients in 2024 across three clinics it runs in Milwaukee. Patients typically lack any health coverage and aren’t asked to pay for their visits.
“We don’t turn anyone away,” Hill Horton said.
But without action from lawmakers in Washington, clinic staff worry that it will become harder to answer every call.
Free clinics like Bread of Healing serve as a final safety net for community members who can’t afford health care. They are bracing for higher demand as more residents are expected to forgo insurance as a crucial tax credit is set to expire and premiums spike.
Affordable Care Act premiums in Wisconsin will increase on average by 17.4 percent next year, a previous Wisconsin Watch analysis showed, with wide variation depending on age, income, family status and geography. Meanwhile, experts estimate more than 270,000 Wisconsinites rely on the enhanced premium tax credit to make insurance more affordable. It will expire at the end of the month without intervention.
People without insurance are less likely to get preventive care. Bread of Healing focuses on treating chronic conditions to prevent people from overwhelming emergency rooms, said executive director Erica Wright.
“If we don’t try our best to move with that demand, we’re not going to be able to see as many people, and there’s going to be a lot of folks falling through the cracks,” she said.
Wright oversees all three Bread of Healing locations. While the clinics have some room to take on more patients right now, she wants to significantly increase their capacity over the next year — adding money and volunteers to serve a possible “monsoon” of demand.
“We’re never going to be able to serve everybody. We know that,” Wright said. “But I don’t want it to be where our phones are ringing off the hook and we just can’t meet at least a good chunk of the demand.”

Marketplace customers face higher premiums and shrinking options
Ashley Bratz paid about $545 a month for a low-deductible marketplace plan this year. When she went to sign up for 2026, that same plan cost over $700.
Even with her job at Open Arms Free Clinic in Walworth County covering a portion of her health care costs, the only option in Bratz’s price range had deductibles higher than what she expects to spend.
“It’s supposed to be reasonable, and this is not reasonable,” Bratz said.
Bratz, who works as the nurse clinic coordinator, said she did not receive enhanced marketplace subsidies this year. Those who did will face a particular shock as the tax credit expires — while also confronting rising prices and shrinking options.
The income-based tax credits have lowered some marketplace enrollees’ monthly premium payments since they became available in 2014.
In 2021, the federal government expanded those subsidies, further bringing costs down for lower-income enrollees and extending smaller subsidies to people making over four times the federal poverty level — $62,600 a year for one person in 2025.
Without an extension, monthly premiums are expected to more than double on average nationally for subsidized enrollees, according to KFF, an independent source for health policy research.
A quarter of enrollees surveyed by KFF said they were “very likely” to go without insurance if their premiums doubled.
The U.S. Senate on Thursday rejected a Democratic plan to extend marketplace subsidies. Republicans, who have long criticized the Affordable Care Act, have instead called for a broader overhaul. The Senate also rejected a Republican plan that would have expanded access to high-deductible insurance plans and deposit $1,000 to $1,500 in enrollees’ health savings accounts — without renewing enhanced subsidies.
Sara Nichols, Open Arms Clinic executive director, is forging ahead regardless. When Bratz told her about her shrinking affordable coverage options, Nichols started working with an insurance broker to find a new plan for the clinic’s small team of paid staff.
“We cannot have health care workers not have health insurance,” Nichols said.
The move left Bratz relieved. Now she’s preparing to help more clients who can’t afford coverage or just need help navigating the complicated system.
They face challenges beyond lost subsidies and premium hikes. President Donald Trump’s “big” bill-turned-law included additional changes to Medicaid funding and the ACA that are expected to increase the number of people without insurance by 10 million over the next decade, according to the Congressional Budget Office.
“We always take what is thrown at us and we figure out how to handle it,” Bratz said. “Do I think we could also use more help? Yes.”
Resources needed to meet demand
Open Arms Free Clinic is already seeing higher demand, Nichols said.
It operates a dental clinic five days a week, and she’s considering whether further demand would require opening its medical clinic for an additional day.
That would take more volunteers and money.
While the Legislature sent state dollars to free clinics in its latest budget, private grants and donations have been harder to secure this year, Nichols said. She expects the clinic will have to get even leaner next year.
But she won’t start turning patients away.
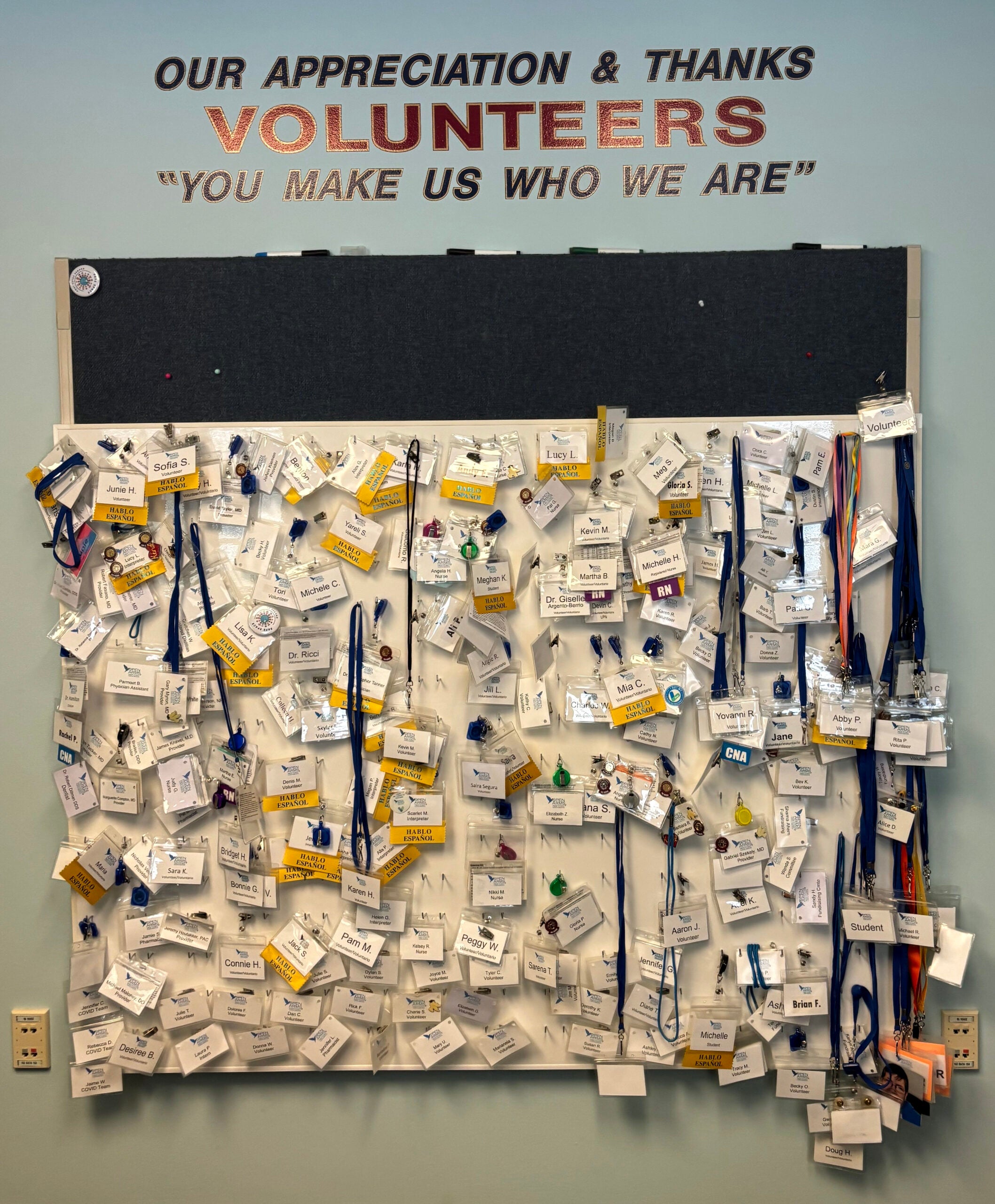
The clinic provides dental, medical and behavioral health to low-income people who live and work in Walworth County. Its 250 volunteers help with things like translating, nursing, greeting patients and connecting people to the clinic. They also provide vision and pharmacy services.
“I know that we have enough smart people and kind people that we’re going to come up with a solution to anything that comes up,” Nichols said.

This is far from the first time Wisconsin’s free clinics have faced big changes, said Dennis Skrajewski, the executive director of the Wisconsin Association of Free and Charitable Clinics.
Free clinics adapted to the COVID-19 pandemic, operating with fewer volunteers and switching to telehealth services and opening vaccine programs, Skrajewski said. Then clinics prepped for increased demand in 2023 after Medicaid unwinding.
“We’re used to waking up and the world changed yesterday, so we’ll adjust,” Skrajewski said.
Wisconsin’s free and charitable clinic association is collaborating with other safety net health providers as part of the Wisconsin Owns Wellbeing initiative, which will host statewide planning meetings to strengthen the state’s safety net services.

Clinic co-founder: ‘I just wish it weren’t needed’
Rick Cesar started working as a parish nurse at Cross Lutheran Church in the 1990s. He took people’s blood pressure at a weekly food pantry and ran an HIV testing site and needle exchange out of the church’s basement.
He helped co-found the Bread of Healing Clinic in 2000, a decade before the ACA passed.
“There were so many people that had no coverage,” Cesar said.
Demand for free services persisted even after more people enrolled in marketplace plans. The clinic expanded to two other locations and hired paid staff. Cesar retired from nursing in 2019 but still regularly volunteers. He feels proud watching the clinic grow.
“I just wish it weren’t needed,” he said.
The clinic is adaptable, Cesar said, whether it’s responding to a pandemic with vaccine drives or helping clients navigate ACA changes.
“We’re going to be here and do as much as we can,” Cesar said. “But those resources, you never know how long they are going to last when the demand is so great.”
Looking for a free clinic?
Find a map of free or charitable clinics near you at wafcclinics.org.