Health insurers often want patients to try the least expensive drug before using more costly or riskier therapies. But this policy can prevent patients from getting the treatment their doctors say they need.
For patients in rural areas, like 30-year-old Samantha Espinosa, having a long drive to the doctor is just one hurdle to getting care. Another is getting the medication she needs. And as Espinosa found out, having health insurance doesn’t necessarily mean you’ll be able to get the therapy your doctor recommends.
Espinosa suffers from psoriasis, a chronic autoimmune disease that caused her to develop tender red sores on her skin and savaged her self-esteem.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
“It was physically painful as well but the emotional pain and now the ongoing scarring is something I’ll have to live with the rest of my life,” she recently said in her New Lisbon home.
In 2012, Espinosa’s doctor prescribed a newer biologic drug to control the psoriasis called Stelara. The drug can cost up to $30,000 a year. Her insurer denied the claim and made her try cheaper steroid creams first. They didn’t work and she still has a large tote bag full of unused medicine.

Samantha Espinosa dumps out leftover steroid creams that were unsuccessful in treating her psoriasis, but were the only medication covered by her insurance company. Shamane Mills/WPR
When the disease was at its worst, more of her body was covered by scaly, itchy patches, than not. One steroid was so potent her husband had to wear gloves when he helped apply it to her body.
“Seth would cover me in one of these tubes on my backside because I couldn’t reach my backside,” she said. “Every move I made my skin would break and crack.”
But creams alone weren’t the end of her nightly ritual. Espinosa had to wrap herself up like a mummy — a technique called occlusion that improves psoriasis.
“We would take Saran Wrap and wrap from my legs up to my neck. So from my neck up I was free of plastic. Everything else was covered,” she explained.

Samantha Espinosa, 30, shows a photo of her legs when her psoriasis — a chronic autoimmune disease — was at its worst. Shamane Mills/WPR
It was uncomfortable but she endured the hassle because she couldn’t take the pills that were covered by her insurance. That medication, methotrexate, might cause liver damage, her doctor said.
State Lawmakers Propose A Change
But now, two state lawmakers are proposing legislation that could help patients get the right medicine with fewer hassles.
“So that one doesn’t have to ‘fail first’ before going on the therapy that the doctor thinks is in the best interests of the patient. Which is really, really important,” said Sen. Alberta Darling, R-River Hills.
The bill’s author in the state Assembly is Rep. John Nygren, R-Marinette.
“This bill provides transparency to a confusing process for patients and doctors,” Nygren said. “It enhances the doctor-patient relationship, expediting necessary care to patients all across Wisconsin.”
Those supporting the change include groups representing patients with chronic, costly conditions like arthritis, cancer, multiple sclerosis, mental health and addiction.
A member of the board of directors for the Wisconsin Society of Addiction Medicine says changes in the bill are “reasonable” and would allow doctors to better tailor treatment to an individual’s situation.
“I have encountered some requirements that made both me and my patient unhappy. It’s very stressful for the patients and very time consuming for (health care) providers,” said Aleksandra Zgierska.
Zgierska’s an associate professor with the University of Wisconsin-Madison School of Medicine and Public Health and is also on the board of the Wisconsin Society of Addiction Medicine.
Zgierska recalled an incident last year in which a pregnant patient suffering from an opioid addiction was treated with buprenorphine. But once she’d delivered the baby, the insurer wouldn’t cover the same treatment.
“It was a big mess,” Zgierska said. “Totally unnecessary medically and this woman went through terrible anxiety, fear that she might be left without the medication (the patient relied on).”
She agrees with the need to control medical costs through what are often called “fail-first” policies, but said all options are not equal and the consequences can be harsh.
“If we have to settle on the second best, or third, or 10th best because of the cost, we are talking about a patient potentially overdosing and dying, that’s a big challenge,” Zgierska said.
So far more than a dozen states have laws overriding step therapy, where a patient must try certain drugs first even if their doctor disagrees.
The proposed Wisconsin legislation would still require pre-authorization for expensive drugs but there would be exemptions and the insurer would have 24 hours to respond to emergency medication requests. If there’s no response during that window, the doctor’s request would automatically be approved.
“That’s really important that we don’t have a patient or provider sitting out in rural Wisconsin or metro Wisconsin, wherever it is, waiting for an answer on whether or not that person can get their medication,” said Angie Thies of the Wisconsin Step Therapy Coalition.

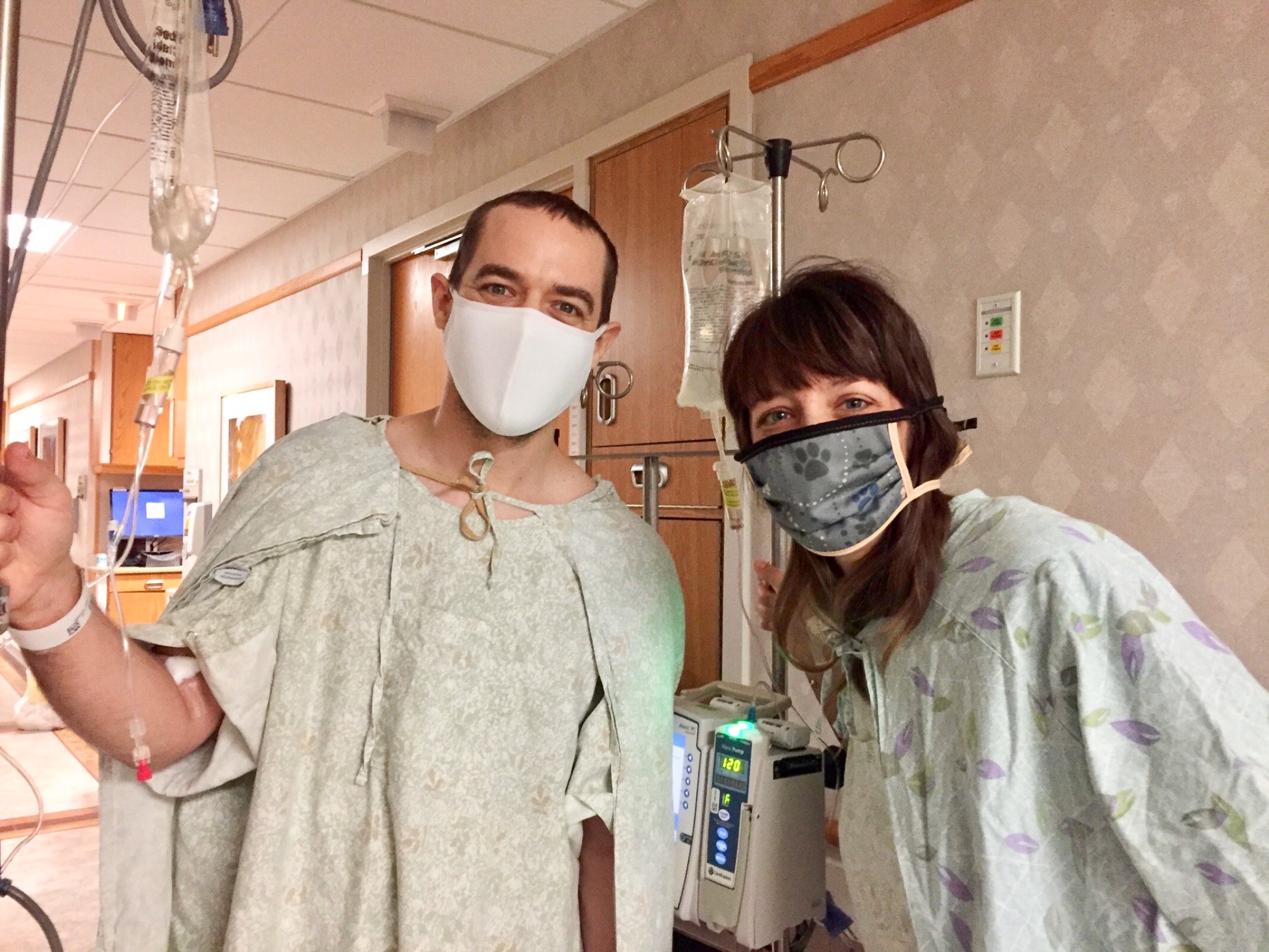
Samantha Espinosa, right, and her husband Seth cook dinner in their New Lisbon home. Espinosa suffers from psoriasis but is doing much better after finally receiving the medication her doctor first recommended. Shamane Mills/WPR
For Espinosa, it took years for her to get the right treatment.
Her psoriasis is now under control because she got the medication originally rejected by her insurer. But the need to keep medical costs in check came at a high personal price. She hopes there’s a better way to balance patients’ needs with skyrocketing prescriptions.
Wisconsin Public Radio, © Copyright 2026, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.