About five years ago, Shawn Wiederhoeft received a life-changing kidney transplant, and in the process, might have helped change the lives of future transplant recipients.
The Madisonian was one of 30 kidney transplant recipients in a recent trial hoping to persuade their body to not reject it’s new organ.
The research, led by a University of Wisconsin-Madison scientist, used stem cells from a patient’s donor to adjust the immune system such that it accepted the new kidney.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
The study, published in the American Journal of Transplantation this month, found the majority of participants who received the treatment were able to wean off burdensome anti-rejection medications for the duration of the study and achieve a better quality of life. Wiederhoeft was one of those people.
The 40-year-old does 3D modeling for a video game studio in Madison. And based on his health today, he said, you wouldn’t know he had a kidney transplant a few years ago.
“It’s so easy to forget that any of that happened,” Wiederhoeft said. “It worked so well that I have to remind myself to be grateful.”
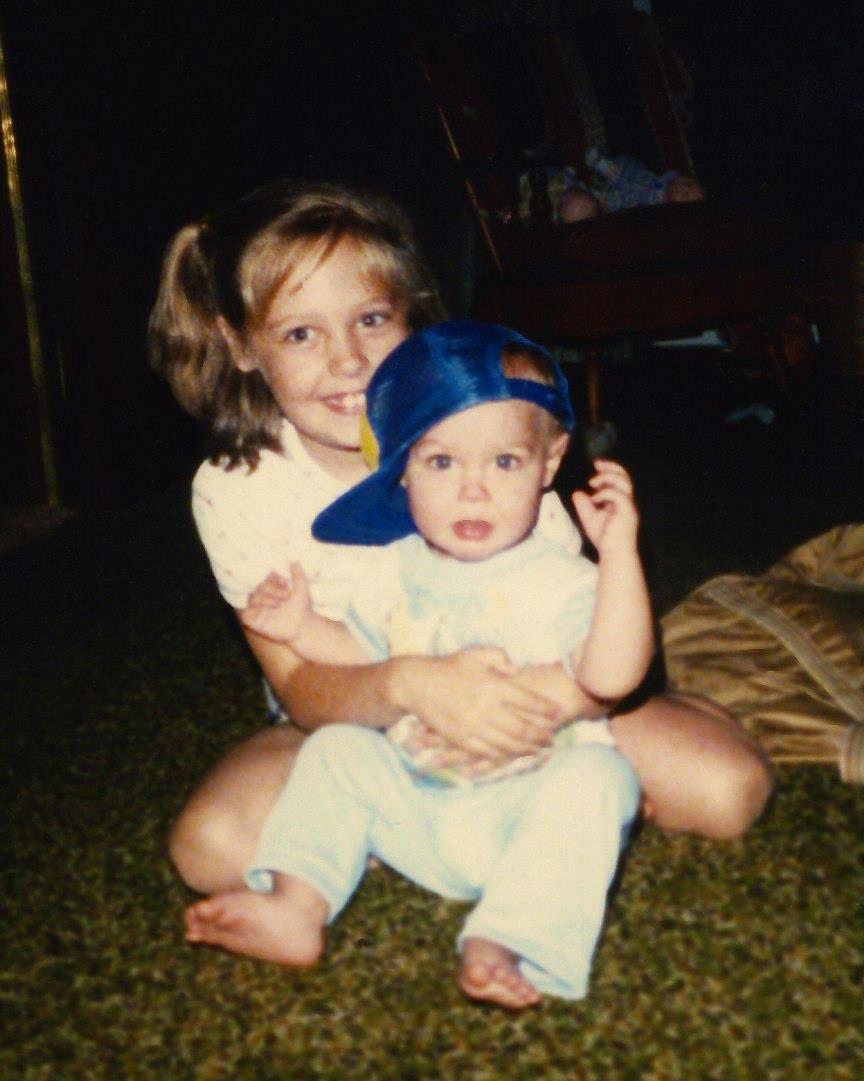
Wiederhoeft had known since high school that he didn’t have fully functioning kidneys, and a transplant might have been inevitable. Then, about seven years ago after routine checkups, his doctor told him it was time. His sister was tested to see if she could donate her kidney to him. Wiederhoeft recalled getting her call.
“She was like: ‘We’re a perfect match, and they told me about this study,’” Wiederhoeft said.
The study was a nationwide Phase 3 trial led by UW-Madison surgery professor Dixon Kaufman. The goal was to test a new stem cell infusion treatment for safety and efficacy. Researchers at 16 U.S. centers and one site in Canada recruited kidney transplant recipients with sibling donors like Wiederhoeft and his sister. They then tested the stem cell treatment on two thirds of patients and followed how they fared compared to participants who followed a routine transplant protocol with ongoing immunosuppressive medication.
“There are many benefits to them (immunosuppressive drugs),” said Kaufman, the medical director of the UW Health Transplant Center. “But of course, there are side effects and downsides.”
Many recipients need to take such anti-rejection medications for life to prevent their bodies from rejecting the new kidney. The drugs can be costly, and ironically, hard on the kidney, Kaufman said.
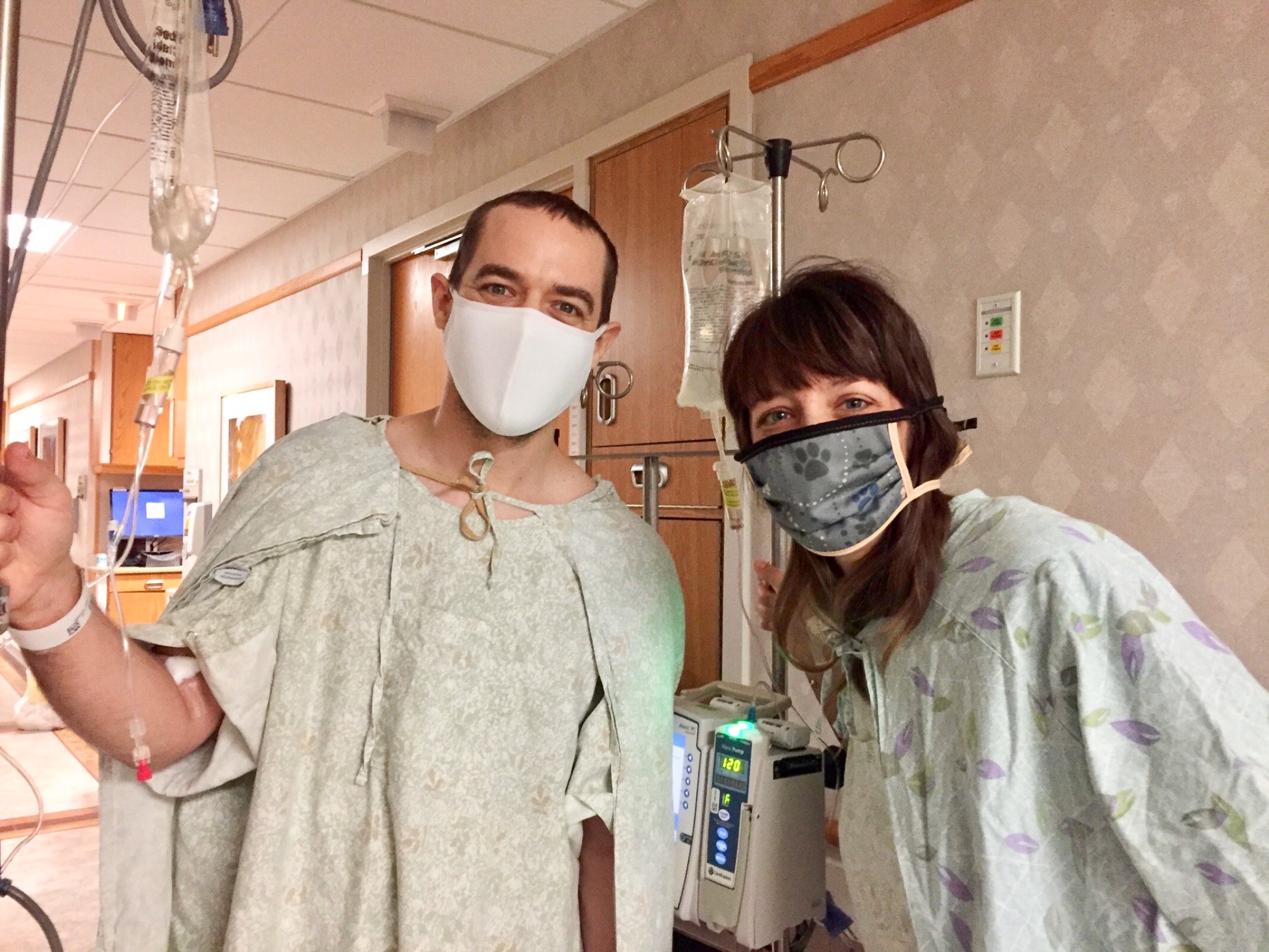
Wiederhoeft got his transplant in 2020. He was on immunosuppressive medication at first.

“I didn’t know all the medications and the potential side effects,” Wiederhoeft said. “From my understanding, they’re like a necessary evil.”
Like other donors in the study, his sister had so-called hematopoietic stem cells removed from her blood. Then, following their live kidney transplant, Wiederhoeft underwent radiation to prepare his body to receive her cells. He later got infusions of her cells.
“So those cells can take hold in the recipient’s bone marrow,” Kaufman said, “and then start to divide and develop into the immune system that reflects that of the donor.”
“That rebalances the immune state of the recipient so that they will not reject the donor organ,” he added.
No more meds
Over time, Wiederhoeft stopped having to take the anti-rejection drugs, with periodic appointments and tests to make sure it was safe to do so.
Today, he said he’s still not on them.
“If you didn’t know any better, there’s no proof that I had to transplant,” Wiederhoeft said.
By the end of the study, 75 percent of patients who received the treatment successfully stopped taking immunosuppressive medication while tolerating their new kidney for the over two years the study monitored them.

The patients who received the stem cell treatment also seemed to have a better overall quality of life compared to those who underwent traditional treatment, according to surveys the researchers administered.
“There was better wellness, quality of life, demonstrated over time in those patients that achieved tolerance and were not taking the medications,” Kaufman said.
Next, the goal is to apply the therapy to transplant pairs who are not perfect matches, like Wiederhoeft and his sister were.
“Unfortunately, (perfect match donations are) just a small proportion of all people undergoing kidney transplantation,” Kaufman said. “It’s harder to do this when you have imperfectly matched donors and recipients. The immune barrier is stronger.”

He also hopes researchers can find a way to apply the therapy to people who are years out from a transplant, or even those who received their kidney from a cadaver.
Wiederhoeft hopes other patients can achieve the ease that he has.
“I feel better than I ever have, even when I was (in) my 20s,” he said. “For both my sister and I … one of the biggest exciting things is the idea that you’re a part of something bigger. And where could this go to help people in the future.”
Wisconsin Public Radio, © Copyright 2026, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.