Marshfield Medical Center family nurse practitioner Brianna Czaikowski says telehealth appointments are a game-changer for some patients. But in serving a mostly rural community, Czaikowski often fights spotty connections and miscommunication when providing virtual care.
“They feel a lot that I’m talking over them, which sometimes I probably am because (of) the delay,” said Czaikowski, a doctor of nursing practice and pediatric urology specialist who sees patients as far away as Michigan’s Upper Peninsula. “You’re not getting that full connection.”
Fresh off a COVID-19 pandemic boom, telehealth is increasingly connecting Wisconsinites living in remote areas to a web of health resources. Telehealth claims in 2020 swelled to a 6.3 percent share of total claims in Wisconsin — an increase of more than 2,400 percent from the previous year, according to a report from the Wisconsin Health Information Organization. Some northern counties reported high gains compared with the rest of the state.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
Helping fuel that growth is the federal government’s COVID-19 Public Health Emergency declaration, which eased regulatory barriers that previously blocked telehealth access. That included relaxing rules for certain prescriptions and changing regulations pertaining to appointments and reimbursement for those on Medicare or Medicaid.
But lingering gaps in broadband access continue to limit services in many rural communities, where telehealth use lags behind better-connected urban communities.
Meanwhile, the federal government ended its emergency declaration in May, leaving questions about how long some telehealth flexibilities will last. Legislation made some changes permanent, but others are set to expire by the end of 2024 or before.
Without action, some of the state’s most vulnerable patients could lose telehealth options they gained during the pandemic.

Pandemic actions expanded telehealth services
After the COVID-19 pandemic struck in March 2020, the Biden administration announced initial telehealth flexibilities that Congress further expanded temporarily — igniting a 63-fold increase in Medicare patients seeking telehealth services that year, according to a federal Department of Health and Human Services report.
Pandemic-era changes, for instance, allowed all eligible Medicare providers to deliver telehealth services that patients could access in their home and outside of previously designated rural areas. The changes waived geographic restrictions on telehealth services and increased options to receive them.
The changes cleared a “huge hurdle” that previously blocked telehealth growth, said Mary DeVany, associate director for the Great Plains Telehealth Resource and Assistance Center.
The pandemic ushered in significant growth for telehealth services for behavioral and mental health. And it has also increased options for certain types of primary care, DeVany said. Remote patient monitoring software, for instance, allows doctors to keep tabs on weight, blood pressure and other vital signs for patients with chronic health conditions, meaning patients with chronic conditions need less frequent hospital or clinic visits.
Telehealth has its limitations. “We can’t see certain things that we could see in the office,” Czaikowski said. That could include immediately spotting signs of child abuse or diagnosing ailments that might not be on a patient’s radar.
But expanded telehealth options have proved “really beneficial” for Czaikowski’s patients in many ways. Although most of her patients still use in-person visits, she said, telehealth visits allow families to check in more often or get simple diagnoses without having to pull their kids out of school and drive long distances for a short in-person visit.
“I see people from Michigan,” Czaikowski said. “They have to drive six hours just to see me. And then to have a 10-minute visit and tell them that their kid is just constipated? Or that they wet the bed — OK, here’s your medicine. That’s a lot for the families to have to give up.”
Health care by phone and Zoom
But not all telehealth options are equal — or accessible to all.
Czaikowski conducts telehealth appointments over video or phone. She prefers video appointments when possible, allowing her to see patients and keep their attention. But she said the majority of telehealth patients she treats rely only on phone calls. That’s in line with national trends among rural patients.
“People will call you from work or when they’re driving and not really give you their full attention,” Czaikowski said. “You have to be really talented in what questions you ask as a provider.”
While phone visits work well for those with less tech literacy or working parents with multiple kids at home, they reduce opportunities for children to communicate health information that parents might not think or want to mention, Czaikowski said.
“The kids tell the truth. When we’re on the (phone) visit, you don’t really hear the kids, it’s more the parent,” she said.

Rural broadband access lags
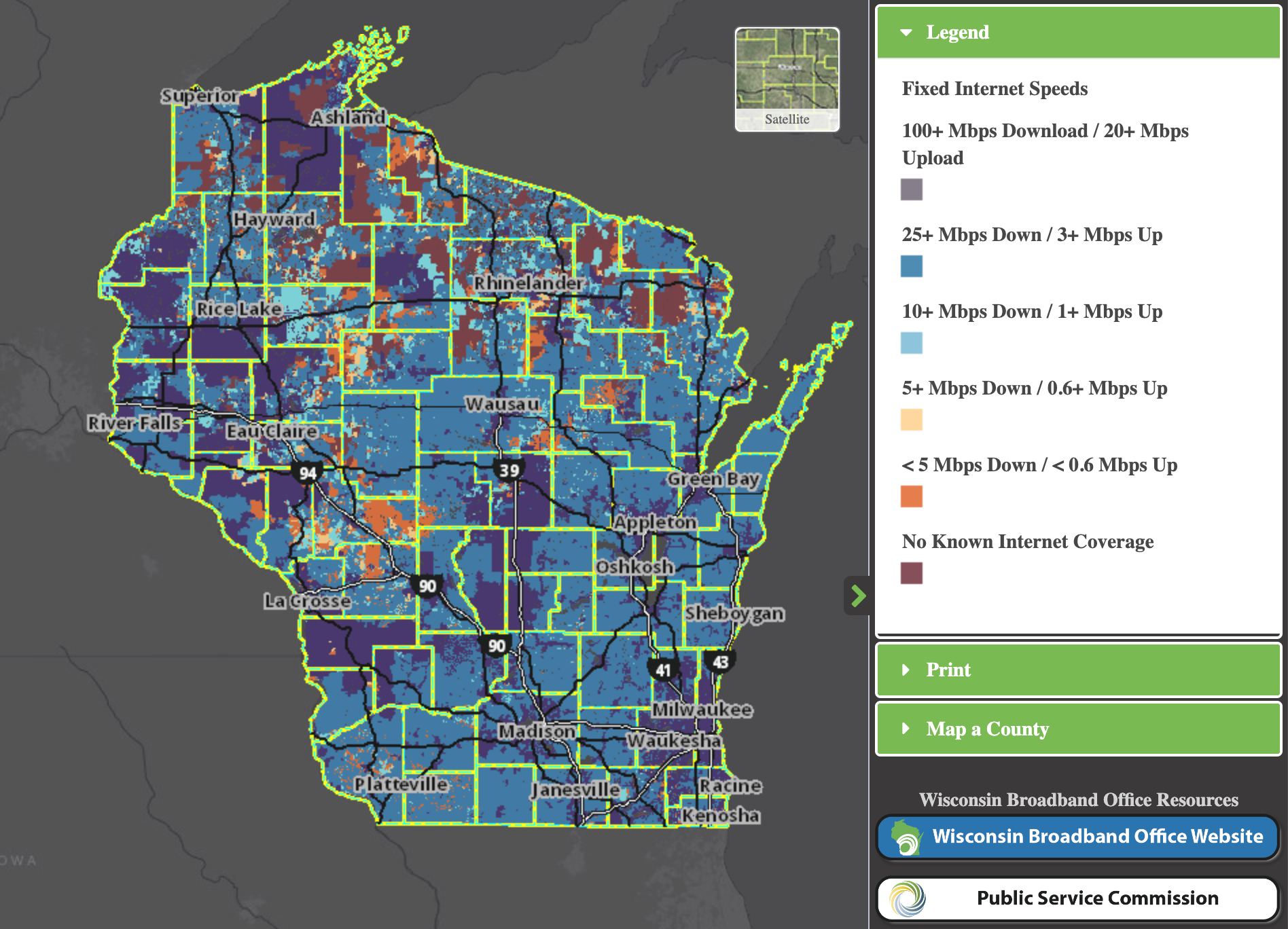
Poor internet service ranks among the top reasons Czaikowski’s patients choose phone appointments over video, which generally should work at download speeds of 25 megabits per second and upload speeds of 3 Mbps — the federal standard for broadband access.
Nearly 22 percent of rural Wisconsinites lack adequate broadband services — a rate far above the rest of the state, according to a 2021 Federal Communications Commission report. And data from the U.S. Census Bureau’s American Community Survey show 38 percent of low-income households in Wisconsin lack an internet subscription.
State leaders are working on solutions.
In 2020 Democratic Gov. Tony Evers established the Governor’s Task Force on Broadband Access, which assists rural communities, many with older populations that want high-quality internet but don’t know where to start.
“They didn’t mind not having broadband, maybe they didn’t see the importance of it,” task force chair Chris Meyer said. “But as their communities age, telehealth suddenly becomes a reason.”
Telecommunications companies find it more lucrative to provide broadband to densely populated urban areas. For-profit businesses happily make the initial, and often heavy, infrastructure investment because they expect to have a large customer base.
But sparsely populated areas are less enticing for private companies. The cost of burying miles of fiber optic cables — one of the fastest and most reliable ways to deliver the internet — can be prohibitive. While a mile of internet service could serve hundreds of homes in a metropolitan area, it would cover only a few homes in northern Wisconsin, Meyer said.
Wisconsin has directed at least $340 million to broadband expansion and connected about 390,000 people to the internet since Evers launched the task force, Meyer said. The state had previously spent about $20 million.
Despite the task force’s increase in spending, Meyer said many people, especially those in northern Wisconsin, have yet to gain high-speed service.
Without broadband access, telehealth is “not a cure-all,” said Kirk Moore, Covering Wisconsin’s navigator who connects northern Wisconsinites to health insurance.
“Just to be able to take on the task of telehealth is a barrier,” Moore said.
Meanwhile, low-income rural Wisconsinites may not make full use of the internet even after fiber optic cables arrive in their communities.
Rural households tend to earn less than urban households in Wisconsin, federal data show. And while a growing share of rural Wisconsinites own a computer, Moore said, “they have a computer but they don’t have the broadband access to be able to hook up to a physician or a behavioral health person through a video.”

Some telehealth flexibilities are temporary
The federal government made some telehealth flexibilities permanent before the emergency declaration ended, particularly for those related to behavioral and mental health. Federally Qualified Health Centers and Rural Health Clinics, for instance, may continue providing such services to Medicare patients without previous geographic restrictions — including over audio-only platforms.
The government has extended similar flexibilities for issues unrelated to behavioral and mental health through only Dec. 31, 2024.
The Drug Enforcement Administration and the Substance Abuse and Mental Health Services Administration additionally extended flexibilities for remote prescriptions of controlled medications, such as treatments for opioid use disorder, through Nov. 11, 2023. The deadline will extend an additional year for new practitioner-patient telemedicine relationships.
Financial incentives affected
The pandemic also affected how hospitals were reimbursed — and financially incentivized — to offer telehealth services.
Under the federal emergency declaration, Medicare and Medicaid in Wisconsin and most other states began reimbursing hospitals for telehealth visits at the same rate as in-person visits.
“That means if you are seen … for something that you would have had covered in person, you are seen for that through telehealth,” DeVany said.
The Wisconsin Department of Health Services in March announced it would permanently reimburse hospitals for most video and audio telehealth services offered to the more than 1 million Wisconsinites on Medicaid — as long as the quality of virtual appointments matched in-person services.
The long-term future of reimbursements for telehealth services through Medicare remains less certain. Without further action, the equal treatment of telehealth and in-person services for billing will expire at the end of 2024.
At that point, Medicare could pay a lower rate for telehealth appointments — excluding the costs of items associated with in-person visits. That would require health care providers to absorb additional costs — or even eliminate services they can’t afford, DeVany said, adding that a similar result could happen with the private insurance market, which often follows Medicare’s lead.
“Once again, the patient would have to come and figure out how to come in,” DeVany said. “It’s a dual-edged sword, in that the patient gets the short end of that deal.”
A bipartisan group of dozens of lawmakers in Congress are pushing to make a range of pandemic-era telehealth flexibilities permanent.
“While telehealth use has skyrocketed these last few years, our laws have not kept up,” U.S. Sen. Brian Schatz, D-Hawaii, said in a June statement. “Telehealth is helping people in every part of the country get the care they need, and it’s here to stay.”
Czaikowski hopes Medicare continues covering telehealth appointments for specialists, which she said are in short supply across Wisconsin. She is among just six nurse practitioners statewide certified in urology, she said.
“They can’t just go to the doctor an hour away. They are traveling six hours,” Czaikowski said about some of her rural patients in Upper Michigan. “I really hope Medicare doesn’t ever take that away because it’s really going to hurt us.”
The nonprofit Wisconsin Watch (www.WisconsinWatch.org) collaborates with WPR, PBS Wisconsin, other news media and the University of Wisconsin-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by Wisconsin Watch do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.