An industry report on hospital and health system finances in Wisconsin shows that services are beginning to approach pre-pandemic levels, but the monetary and health effects of canceled or delayed medical care are “significant.”
Early last year, some surgeries and medical screenings were put off as hospitals prepared for a surge in COVID-19 patients and tried to stop the spread of the virus. Outpatient procedures and surgeries were down 45 percent during three months in 2020 compared to 2019, according to a report by the Wisconsin Hospital Association.
Many hospitals shut down non-emergent care from April through June last year at the urging of the U.S. Department of Health and Human Services. Declining revenue led some hospitals to furlough staff.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
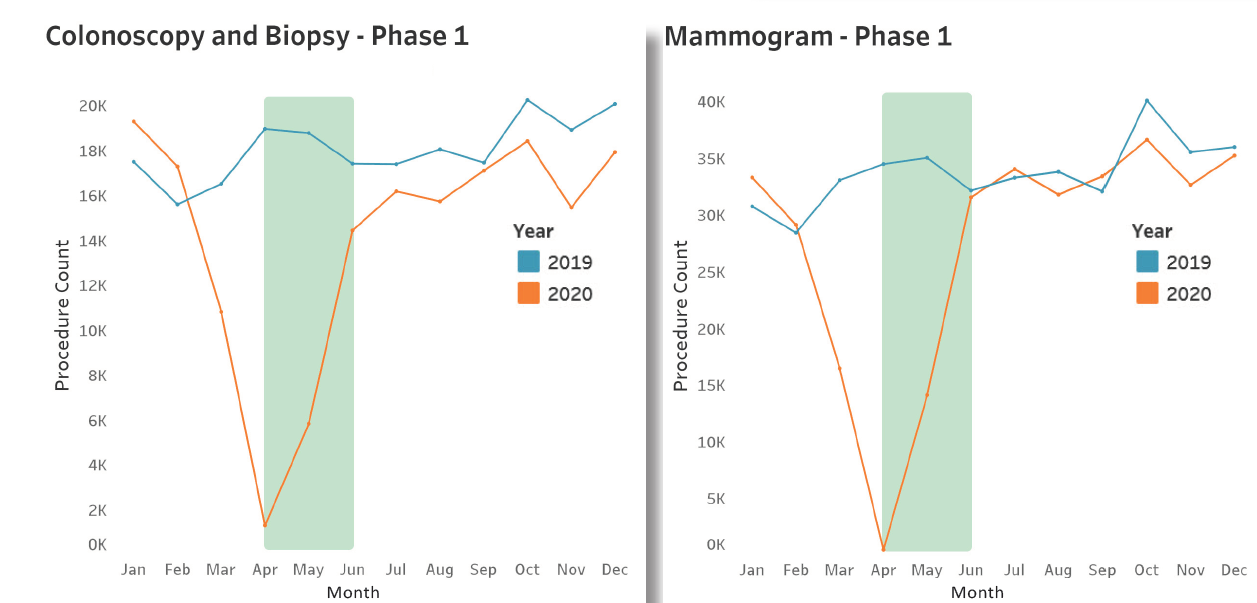
During summer and early fall, medical care in Wisconsin rebounded, but not to 2019 levels, even though former U.S. Health and Human Services Secretary and longtime Wisconsin Gov. Tommy Thompson urged people not to put off needed care in a public service announcement.
Routine medical care was later “crowded out” from October to December as coronavirus cases surged in the state and 76 hospitals of 140 reached peak capacity, said Brian Potter, vice president of finance for the Wisconsin Hospital Association.
While some financial gains can be attributed to returning patient volumes, the impacts of the pandemic are far from over, according to an assessment by health care consulting firm Kaufman Hall.
It predicts one-third to one-half of U.S. hospitals may have negative operating margins by the end of the year as a result.
That assessment by Kaufman Hall forecasts the lingering effects of COVID-19 could drive 2021 hospital margins down 10 percent to 80 percent, and 2021 revenues down $53-$122 billion compared to pre-pandemic levels.
But some are skeptical that hospital bottom lines will suffer to that degree.
“These are institutions that have piled up, most of them non-profit, huge margins year after year, built up huge reserves. They’re supposed to be able to handle a pandemic without claiming they’re impoverished,” said executive director of Citizen Action of Wisconsin Robert Kraig.
WHA’s Potter said the revenue hit for Wisconsin hospitals was $2.5 billion early in the pandemic. That was partially offset by federal money from the coronavirus relief package, known as the CARES Act.
“It wasn’t like the CARES dollars made up for those revenue losses. But they were certainly necessary and very helpful,” said Potter. “But it’s hard to know how that’s ultimately going to affect margins.”
An examination of financial records by Kaiser Health News shows some hospitals around the country recouped pandemic losses and even thrived because of the federal bailout.
Wisconsin Public Radio, © Copyright 2026, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.





