The world has been hit with an unprecedented health care crisis not seen since the flu pandemic of 1918 and an economic challenge comparable to the Great Depression.
In Wisconsin, Milwaukee was hit the hardest with COVID-19 early on. With cases doubling less than every three days.
Over time, Milwaukee has stretched that to more than 18 days whereas the rest of the state is seeing faster growth in their infection rates, and doubling times of about 14 days.
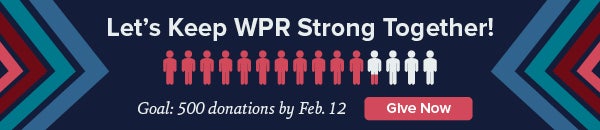
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
“We have a lot of evidence we’ve at least hit an equilibrium with COVID-19 here in Milwaukee,” said Dr. John Raymond, president and CEO of the Medical College of Wisconsin. “We have flattened the curve very effectively, we have not smashed the curve. We haven’t extinguished COVID-19 and it’s very likely until we find a vaccine, we are going to have to learn to live with it.”
WPR’s Corrinne Hess recently spoke with Raymond, Milwaukee Mayor Tom Barrett and Dr. Ben Weston, medical director of the Milwaukee County Office of Emergency Management, about the lessons they’ve learned over the last eight weeks since the COVID-19 pandemic struck Milwaukee County and Wisconsin.
These interviews have been edited for brevity and clarity.
Q: What is your biggest takeaway so far in dealing with this crisis?
Milwaukee Mayor Tom Barrett: Nationally, there was such a shortage of tests it was very, very frustrating we could not do more testing. Clearly, other parts of the state are going to benefit because there is much more testing available now. And in some instances the issue isn’t going to be testing availability, it’s going to be having people actually take the test. My advice would be test, test, test as much as you can.
Dr. John Raymond: Clearly going forward we need to invest a lot more in our public health infrastructure. And in Milwaukee County, it doesn’t make sense to have 11 different municipal public health departments. There needs to be a lot more local coordination, if not more statewide and federally.
I also think we need to significantly diversify our clinical revenue base. One thing we always knew, but has now really confronted us, is that the system is much too dependent on procedural income that subsidizes all of what we do.
Our supply chain is fragile. We might need to re-examine the just-in-time philosophy we have with our supply chain and perhaps rely more on local vendors rather than have an international supply chain.
Dr. Ben Weston: Information keeps changing, and we keep learning more every single day because it is a novel coronavirus. The greatest learning point locally has been collaboration and using that collaboration to plan for the future.
We have 11 different public health departments, 15 fire departments, multiple mayors, five hospital systems. There is a lot of — by design — fragmentation. When something like this happens, we have to pull together. The fire departments were the first to pull together and then the others followed suit.
If we stayed individualized and everyone came up with their own policies and procedures, it would have confused each of us, it would have exasperated the pandemic, and it would have confused the public as well.
Q: More tests are available now, why is this so important?
Barrett: If you can identify the people who have tested positive, if you can quarantine them, if you can then reach the contacts that they’ve had, that to me is the key to containing the disease and the key to actually reopening the economy.
First and foremost we want to make sure people are not infecting other people. But we also need to do a better job of getting a baseline of people who live in the state of Wisconsin. Right now, we have probably only tested 1 percent of people, that is not enough to build a structure that will allow us to contain the disease moving forward.
Weston: There are number of reasons. One is so we can get an idea of the true burden of COVID-19 in our community. And if you test more, you can hone in on certain elements. What is the true death rate? What is the true hospitalization rate? How many people are truly symptomatic when they get the disease? The more people you test the more data you have.
The other reason it’s really important to test now is as we move into the next phase and start to pull back the stay-at-home order, we need to have testing in place because we know we are just at the beginning and there will be more outbreaks, not just in facility settings but in communities.
Q: What question do you get asked most by people in the community?
Barrett: We still get a lot of questions about testing. It is available now for people who are symptomatic. Ultimately, we will get to the stage for people who are not symptomatic.
Raymond: People are concerned about their safety at work. But also concerned about their livelihood and needing to put food on the table. I think people are troubled by the political overtones and the incivility and this difficult balance we are having between our health and our economy.
Weston: What’s next? It’s a great question and an important question. We are preparing. We didn’t know how well social distancing was going to work. It looks like it has been fairly successful. We didn’t see the overwhelming surge to our ambulance system, to our 911 system, to our hospital system, that was feared. And that’s because of social distancing.
To be honest, we know this is just the beginning of COVID-19 in our community. The peak we have seen may very well not be the worst we see until a vaccine is developed. So we are in this for the long haul. But I think we have put together an infrastructure that can get us through this.
Q: What should people in your position in communities outside of Milwaukee know as coronavirus cases increase across Wisconsin?
Barrett: I think the fact that we’ve been at this for eight weeks provides a road map for some other communities.
Some of the biggest barriers have been overcome because of Gov. Tony Evers’ actions, for example closing bars and restaurants right before St. Patrick’s Day. And I say that being cognizant of the fact that before the (state) Supreme Court and state legislators there is a real concern of how much easing there is going to be.
Weston: Take a look at other communities that have had more cases and more deaths. What have they done? For better or worse, there are a lot of communities to look at and see what went well and what didn’t go well.
Q: What should have been done differently locally?
Raymond: Obviously it’s easy to look back and second guess, but I think in Milwaukee and at the state level, we’ve done a very good job. Inarguably, Wisconsin has had among the very best results in the Midwest, especially when you compare us to Illinois, Michigan, Indiana and Iowa. “Safer at Home” has worked. It was implemented relatively quickly and effectively with bipartisan support.
I do wish we would have had the foresight to intervene more quickly in African American and Latino communities. And maybe we should have focused a little earlier on mitigation in long-term care facilities, nursing homes and food-processing plants, but again, it’s easy to look back and say, “We coulda, shoulda, woulda done better.”
Weston: One thing that can always be done better is to try to reach everyone with messaging. We can do as much as we want with building up plans and procedures, but if we don’t message how important it is to stay at home, social distance, minimize trips, then everything we do is somewhat of a waste.
Q: What about nationally?
Barrett: I think public health experts, politicians and historians will be debating this for years. I don’t want to say it’s water over the damn, but right now I don’t have the luxury to say, “Let’s do a post-game analysis.” It’s not over yet. It’s a life and death issue.
I think at some point we’ll look at what went wrong. Our country has had so many cases here. So many more deaths here. We should have handled in a much different way. Right now, our emphasis should be on how do we continue to navigate these difficult waters.
Raymond: Again, it’s easy to speculate what we could have done better. Our nation could have done much better by earlier and more stringent travel restrictions and a coordinated national lock-down policy. Another national shortfall has been states, municipalities and health care systems having to compete for testing, personal protective equipment (PPE), ventilators and, in some cases, even talent.
Weston: Earlier recognition. When you compare the U.S. to South Korea, the recognition and mobilization of resources like PPE and ventilators is dramatically different.
Q: Looking ahead, what can we expect?
Raymond: The pandemic has forced us to look at how to do things very differently. How to perform virtual visits and tele-education that we knew we might need to do but never had the urgency to implement, and I think that will benefit us going forward.
I expect as we relax some of the workplace restrictions going forward, whether that comes from a (state) Supreme Court decision, or phasing in through the “Badger Bounce Back” plan, we’re going to see more cases of COVID-19.
If there aren’t travel restrictions, all it takes is one person to start a chain or spread of the disease in another community.
Wisconsin Public Radio, © Copyright 2026, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.