COVID-19 infection rates have been increasing throughout the summer. One epidemiologist is advocating for getting booster shots now to target recent variants in hopes of avoiding another spike as Wisconsin edges into respiratory virus season.
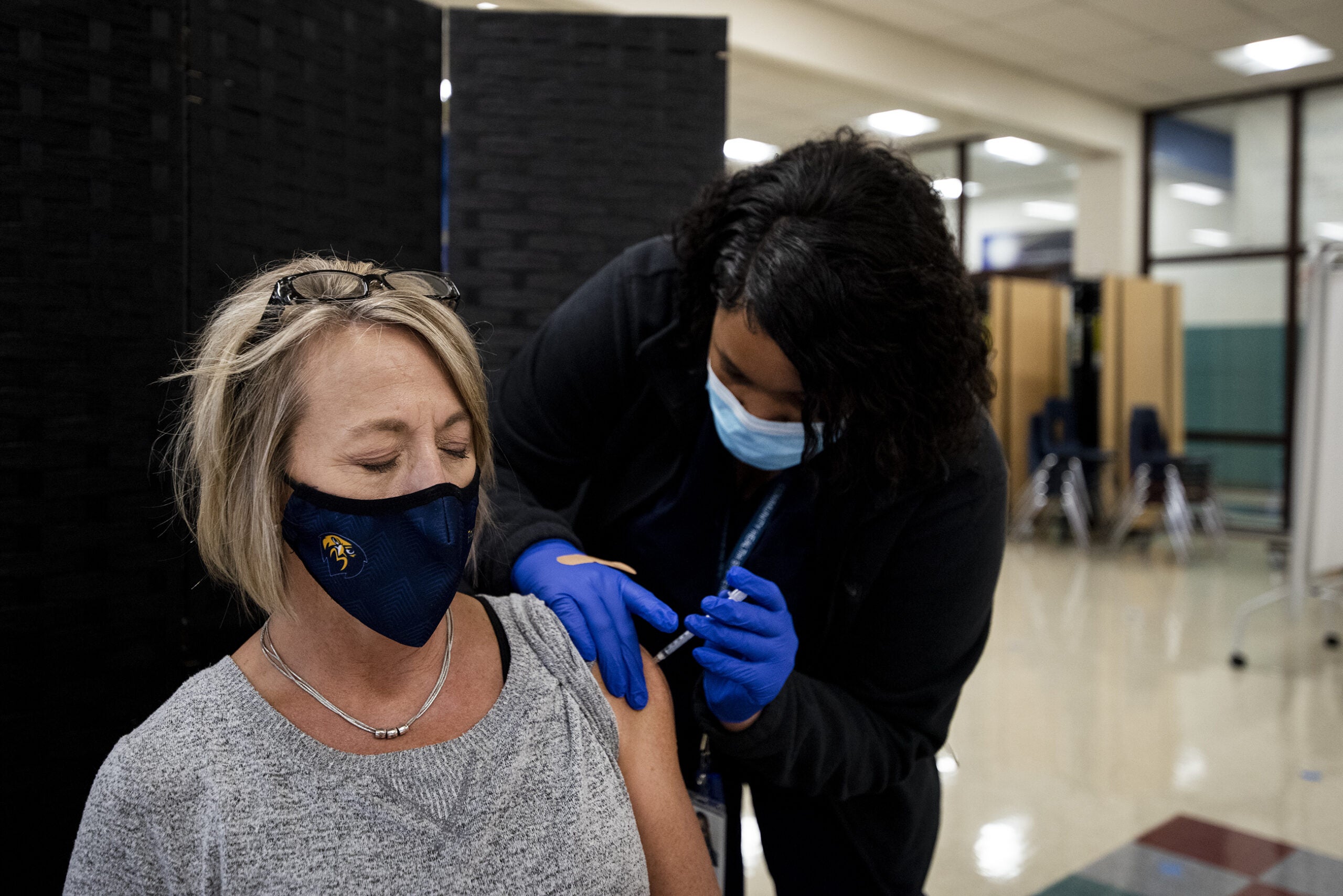
The Centers for Disease Control and Prevention recently recommended people ages 6 months and older get an updated COVID-19 booster. Anyone 5 years and older should get one vaccine at least two months out from receiving any other COVID-19 vaccination, according to the CDC. Those 6 months to 4 years old may get more than one updated vaccine to be considered up-to-date, depending on how they were previously vaccinated.
Ajay Sethi, professor of population health sciences at the University of Wisconsin-Madison and an infectious disease epidemiologist, joined Wisconsin Public Radio’s “The Larry Meiller Show” to provide an update on COVID-19, recent variants and vaccines that target them.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
“It’s not a bad idea to get updated with a vaccine that targets the most recent variants. But if you’ve had COVID recently, I understand why people would opt to not get the booster immediately. But at some point, it’s something you ought to consider,” he said.
This interview has been edited for clarity and brevity.
Larry Meiller: As we head into the cooler months, what do we know about COVID infection rates during fall and winter months?
AS: They’ve been kind of climbing all summer. When school was let out back in June, people were traveling and gathering and doing the kinds of things we do in the summer. And because of that heat dome we all experienced, people also went inside to seek air conditioning.
We’ve been seeing this increase in COVID transmission all summer, and now the fall is upon us. School’s back in session. And with this time of year, we begin respiratory virus season. So COVID continues to climb. And what’s worrying is that hospitalizations are climbing as well. Deaths are not, but they are higher than we’d like.
LM: COVID’s mutated many times. Why do viruses mutate?
AS: Viruses have opportunities to mutate because they replicate at high levels. And viruses, whose genetic material is RNA, tend to mutate more than other types of viruses. And that’s the case with SARS-CoV-2. It definitely evolves faster than we appreciated when it first emerged. But now it’s understood.
And tracking those variants is helpful so that we can become aware of any variants that may escape the immunity we already have in our communities to the point where we’d want to think about some other strategy.
But for now, the variants that circulate can be mostly handled by our immunity, but not for everybody.

LM: Well, two of the latest variants — EG.5 and BA.2.86 — what do people need to know about these variants?
AS: For both of those, plus all the variants that you can see on the CDC tracker webpage, they’re all of the omicron family. And on top of that, all of the variants are either in the XBB lineage or an offshoot of XBB.
The BA.2.86 isn’t on the CDC tracker because there are just a handful of cases that have been picked up through surveillance around the country. It got everybody’s attention because it has a lot of mutations — 30 plus mutations. But as it turns out, laboratory studies have shown that the immunity that’s already out there, the immunity that will be generated from the upcoming booster, can handle BA.2.86.
EG.5 represents the virus that’s of highest proportion. About 21.5 percent of viruses are of this type, but it doesn’t represent something that’s so different from what our antibodies can recognize.
LM: If somebody got, let’s say, that extra booster shot that was offered in the summer, it’s a different shot than the new shot, right?
AS: Yeah. The boosters that have been in use so far have been the bivalent booster. And a year ago is when they came out. And the thinking was that you want to stimulate a little bit of the immunity you already have by including the original strain of the virus that was in the vaccines that were first released and used. And then you want to include a little bit of the RNA representing the virus that was circulating at a time.
Now we want to update that. But we’ve stripped away that ancestral strain of the virus from the vaccine. So it’s now monovalent, and it’s only going to contain the virus that’s currently circulating. It’s based on XBB.1.15. It doesn’t represent the highest proportion of viruses that are out there, but all of the viruses that are circulating right now are of the XBB lineage or an offshoot of it.
LM: How likely is it that COVID shots will become like the flu shot — regular and seasonal?
AS: I guess we’ll find out in a couple of years if this really does become the strategy. I think right now the biggest concern is the virus evolves faster than we could sort of keep up with them.
So when it was decided that XBB.1.15 was going to be the virus of choice to target for this booster, new variants almost immediately came out, raising alarm bells. And it turns out we can handle those new variants. So I think it’ll be an annual thing, probably. But we have to also have some confidence that what’s being produced will be effective. And I think that is still something we have to learn more about.
LM: How much should the general public worry about COVID?
AS: For most people, COVID turns out to be mild. But long COVID is something we should always be aware of.
I’ll say that roughly 3 percent of our country is living with moderately or severe immunocompromised states. Those individuals are at risk for severe disease and death from COVID. So although the emergency declaration is over, the pandemic continues for everybody.
Last year, COVID was the number three cause of death in the United States. And it’s been a long time since an infectious disease was in the top ten or the top five causes of death in the United States. So it’s still very concerning.
LM: Is there some indication of how effective this new vaccine is and how long this effectiveness might last?
AS: The antibodies in the blood will wane after four to six months. You still have immunity from vaccination for a later time period, but the antibodies will take a little bit — a few days — to kick in when you do get infected.
What you want to avoid is to have that initial course of illness, which can sometimes get a little severe. You also want antibodies that are matched with what’s circulating. So the vaccines do have a longer term benefit, but definitely four to six months is where we have measurable antibodies in the blood after vaccination.
Other things to know from Ajay Sethi:
- On Novavax: The FDA approved boosters that are produced by Moderna and Pfizer, but not Novavax, though that may come in the future. Novavax uses a more familiar technology that’s been in use for a while for vaccines. It has merit in that it may be more likely to encourage people to get vaccinated if they have any concerns about an RNA vaccine because the Novavax vaccine is a protein vaccine. But at this point, options for the updated booster are ones by Moderna and Pfizer.
- On switching between vaccine brands: Some small studies have shown it might be good to switch off between Moderna and Pfizer vaccines. The amount of virus RNA in each of the vaccines is a little bit different — Moderna has a bit more than Pfizer — but as far as the CDC and FDA are concerned, the vaccines are interchangeable. It’s best to get whichever one is available to you.
- On which arm to use: Another study showed that getting the vaccine in the same arm could help stimulate immune cells that are still hanging around the area from your previous shot, which could help spur on a better immune response the second time around, compared to switching arms.
- On sequence of vaccines: Even if you missed some doses, you can get the new one. Talk to your doctor to confirm, but that’s the recommendation.
Wisconsin Public Radio, © Copyright 2026, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.