An immune response to the COVID-19 vaccine that presents similarly to a symptom of breast cancer can be alarming for some mammography patients, but medical experts say there’s no immediate cause for concern.
Swollen lymph nodes near the armpit can be a sign of breast cancer. And up to 16 percent of people who receive the COVID-19 vaccine report feeling tenderness near their armpits, said Dr. Roberta Strigel, chief of Breast Imaging and Intervention for the Department of Radiology at UW Health.
“That’s the body’s normal response to the vaccine,” Strigel said of the swollen lymph nodes. “It doesn’t happen in everyone, but if it does happen, it’s an expected response to the vaccine.”
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
Some people may feel tenderness, and others might experience a lump on the side where they received the vaccine. Others may have swollen lymph nodes but might not notice.
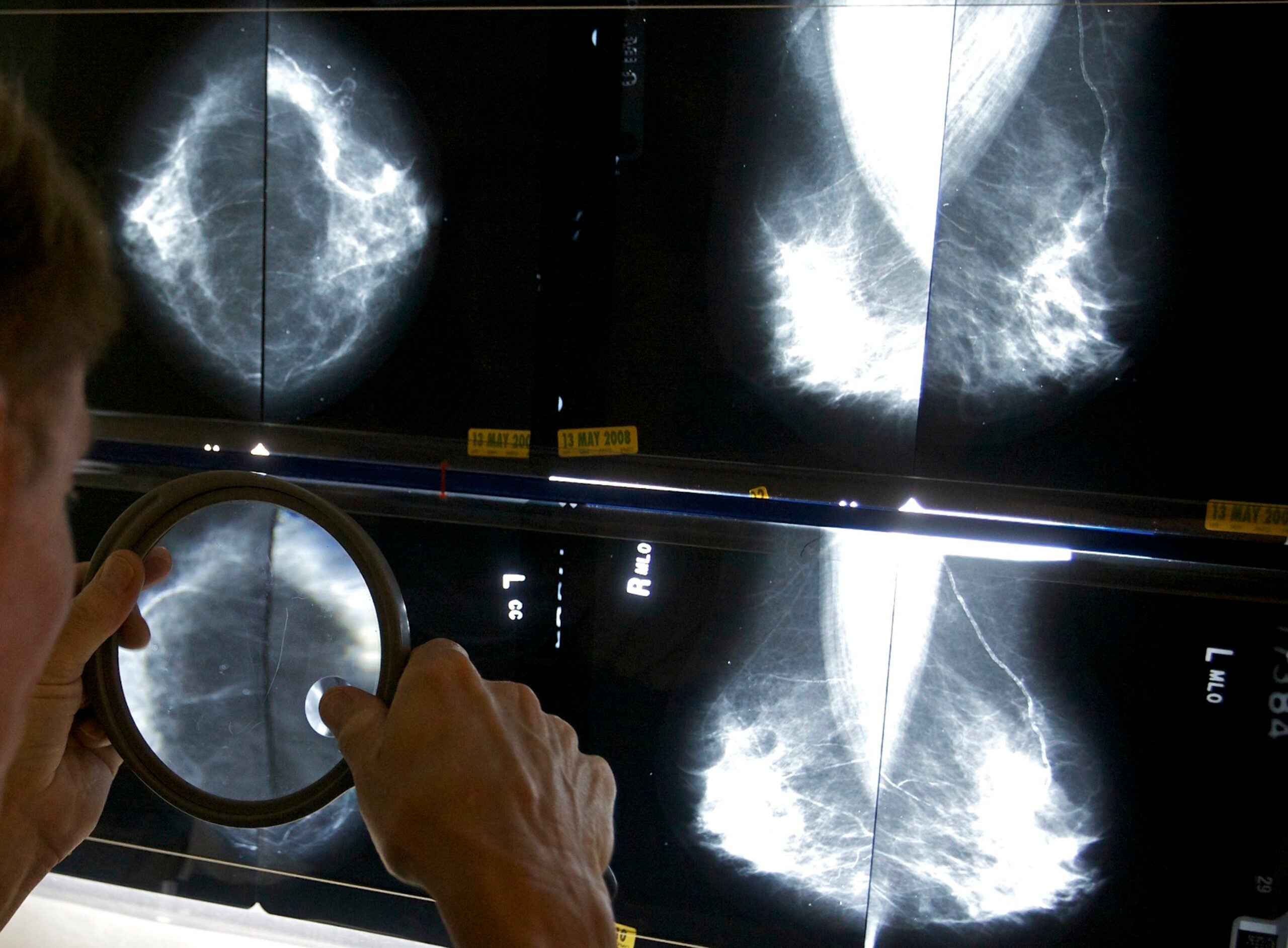
That’s causing concern for some people during mammography exams, especially because swollen lymph nodes can be seen on the mammogram.
To ensure that the swollen lymph nodes are related to the vaccine and not to breast cancer, Strigel said patients could opt to wait four to six weeks after receiving the vaccine before going in for a mammography.
“If (the patient) does have some swelling of the lymph nodes, we expect it to resolve by then,” she said.
Strigel warned that if a patient is overdue for a screening, it’s best not to delay it. She said health experts are concerned now about a decline that’s been witnessed in cancer screening and subsequently cancer diagnoses.
“If we look at breast cancer, for example, we know that not as many people were diagnosed with breast cancer in the last year, but we know those cancers are out there,” she said.
Strigel suspects patients delayed screenings because of COVID-19, either because appointments were canceled or because patients were nervous about being in a health care facility during the pandemic.
Strigel said many mechanisms are in place at the facility to make it safe for all patients, including those who need preventative exams.
At UW Health Breast Center, patients who come in for mammograms should expect to answer the following questions: have you had the COVID-19 vaccine; what arm was it delivered to; and what date did you get the vaccine?
“Then, when I’m looking at a mammogram, if I see lymph nodes that are swollen, then I know that is likely the cause in many people,” Strigel said. “So that’s really helpful to us.”
She advised volunteering that information if the medical experts don’t ask for it.
For patients who have a history of breast cancer, Strigel advised that they get the vaccine in the arm opposite the side where the cancer was detected.
“When we read a mammogram on the side of cancer, and really on both sides, we’re always looking for changes,” she said. “Is there a change in the breast and is there a change in the lymph nodes? So it’s helpful to us to have the vaccination on the opposite arm, if that’s possible.”
Strigel said if she screens a patient with swollen lymph nodes on the side where the vaccine was administered, she may opt against doing more imaging.
However, if swollen lymph nodes appear on the side opposite to where the vaccine was given, and especially if there’s a history of cancer, she would likely call for diagnostic imaging, which gives providers more information to understand what’s happening inside the breast.
Mammography exams are recommended for women starting at age 40. Some patients may need imaging sooner if they’re at higher risk for breast cancer. Strigel said it’s best to talk with your provider about preferences for screening.
Wisconsin Public Radio, © Copyright 2026, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.