The decision by federal regulators to approve COVID-19 booster shots reassured those wondering whether they were as protected from the disease as they could be. But the news has prompted even more questions and sometimes confusion about who can get a shot, what it does or doesn’t prevent, and whether it will interfere with other vaccines.
Several people reached out to WPR’s WHYsconsin asking a range of questions about booster shots, here is what we learned.
Can everyone get a booster shot? Does it depend on which brand of shot you got originally?
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
At this time, the Pfizer booster authorization only applies to people who received the Pfizer vaccine initially. Those who got the Moderna or Johnson & Johnson vaccine will likely need a booster shot in the near future, but regulators are waiting for more data which could come soon, according to the Wisconsin Department of Health Services.
Who is eligible for booster shot is narrowed down even further according to age, medical condition and other risk factors such as whether your job or where you live increases exposure to COVID-19.
People that should get a shot include those over age 65, residents of long-term care and people age 50 to 64 with certain medical conditions.
Those who may get a shot six months after receiving their second dose of Pfizer vaccine include first responders, teachers, postal workers and other frontline workers according to a list DHS said could grow.
Does an additional shot protect against long COVID-19?
Because long COVID-19 is chronic and occurs over a longer period of time than symptoms from the initial infection, it will take time for there to be enough scientific data to say for certain whether a booster is of benefit in also preventing potential long-term complications from COVID-19.
At this point, there is preliminary data that long-haul COVID-19 is less likely to occur in vaccinated individuals compared to the unvaccinated, said UW Health’s Dr. Joe McBride. He stressed that research is ongoing and that it’s important people get their first and second shots of the vaccine.
“I think most Wisconsinites would want to know, ‘Am I doing what I can to prevent against serious illness in myself’ and then also helping my community by getting vaccinated. And the answer is yes,’” he said.
Can I get a COVID-19 booster and a flu shot?
The Centers for Disease Control and Prevention says you no longer need to wait any time between getting a COVID-19 vaccine and any other vaccines, including the flu shot. You can get them on the same day, according to advice the agency gives to doctors.
Some Wisconsin health systems have urged patients to contact their doctor for a flu shot and to schedule a COVID-19 booster shot if they’re eligible.
“I do think there’s going to be different ways to make it simple and convenient for people to get these vaccines and I do think there’s going to be a number of drive-thru locations that will start up soon,” said Dr. James Conway of the University of Wisconsin-Madison’s Global Health Institute.
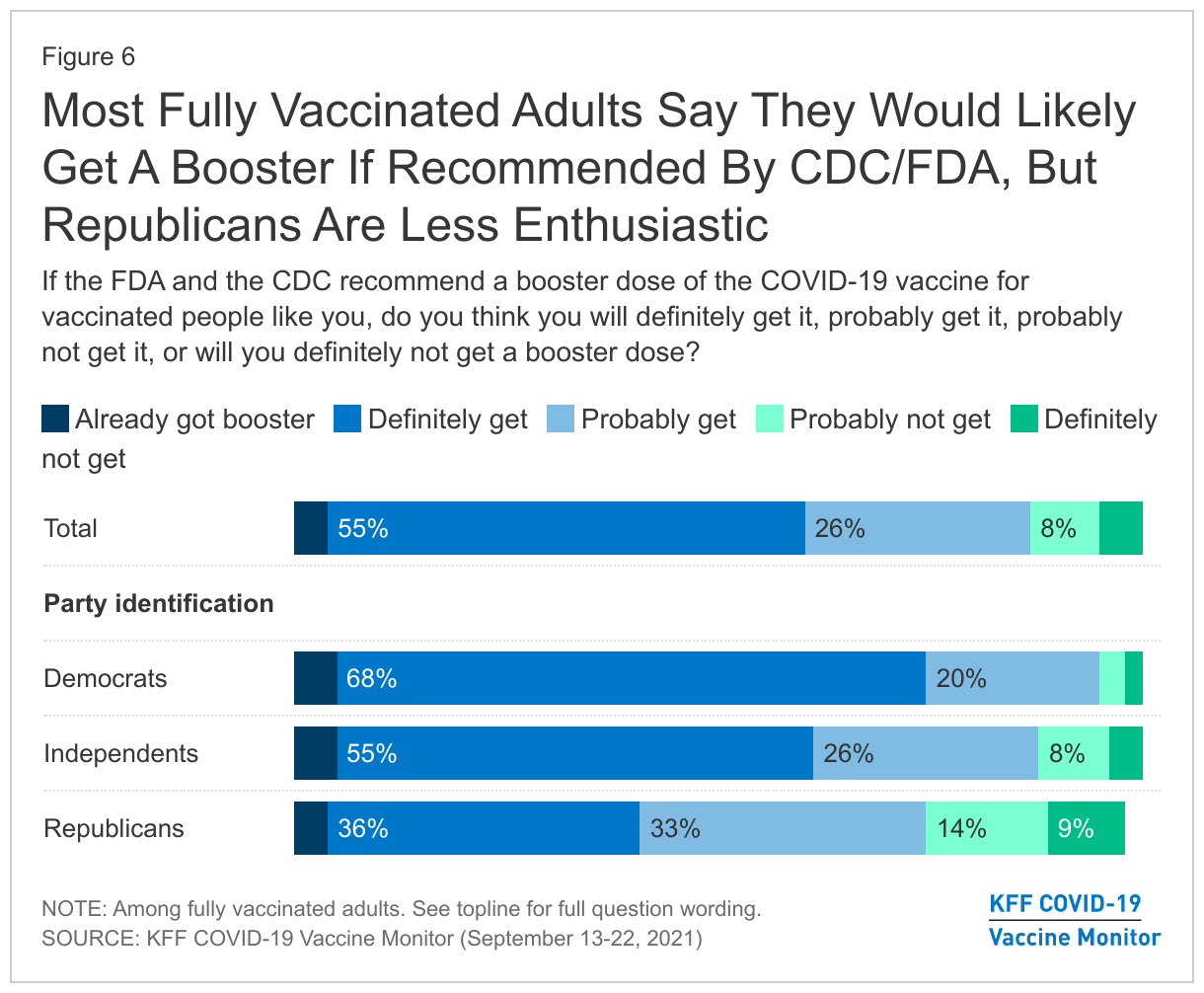
We know who can get a booster, but how many will actually follow through?
According to a new national poll by the Kaiser Family Foundation, more than three-quarters of those asked said they will get a booster if the CDC has recommended it for them.
However, the poll finds there is a partisan gap. Democrats are almost twice as likely as Republicans to say they’ll “definitely” get a booster.
Why is a booster needed if the vaccines are so effective?
All three vaccines were found to give high protection against disease and hospitalization.
In the case of the Pfizer vaccine, it was found to be 95 percent effective against severe disease. But no vaccine is 100 percent effective and there have been breakthrough cases where immunized people become infected, hospitalized or even die — although death after vaccination is extremely rare.
Current data from DHS shows those who are unvaccinated are 4 times more likely to contract COVID-19, 9 times more likely to be hospitalized and 11 times more likely to die from the virus than those who are fully vaccinated.
The reason immunized people sometimes get infected has to do with many factors. All vaccines lose protection over time. The delta variant of the coronavirus is highly contagious, and Wisconsin’s population is older, so is overall more susceptible to disease. In addition, the vaccines had strict storage and handling requirements which may not have always been followed, lowering their efficacy.
“What’s at play here are multiple variables that have proven very difficult to tease apart one from the other, to say ‘It’s this, not that factor,’” said Dr. Gregory Poland, an infectious disease expert and head of the Mayo Clinic’s Vaccine Research Group.