The Food and Drug Administration on Nov. 10 stopped requiring warning labels on a range of hormone therapy treatments for women experiencing menopause and perimenopause symptoms.
“It was a monumental day, honestly, for women and for women’s health,” said Dr. Tes Jordens, a physician whose telemedicine practice, 1988 Wellness, focuses on Wisconsin women going through menopause.
Black box safety labels on menopausal hormone therapy, including topical estrogen creams, were removed to reflect current scientific evidence that they are safe. Jordens recently told WPR’s “The Larry Meiller Show” that the labels erroneously suggested that use of these medications increased the risk of breast cancer, heart disease, strokes and dementia.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
“That’s just frankly not true,” Jordens said. “It doesn’t have any systemic effects and has never been shown to have any of these risks.”
“I’m hopeful physicians and other providers will see this and feel better about prescribing or learning about what these resources are, and not turn away woman who are asking for that kind of help,” she added.
In her practice, Jordens aids women with a myriad of menopausal symptoms by recommending dietary changes, movement and hormone therapy.
“It’s not about just symptoms,” she said. “It’s educating women about how certain lifestyle choices, medications or both can increase their life span, avoid chronic diseases further down the road and get them to be the healthiest versions of themselves.”
The following interview was edited for brevity and clarity.
Jill Nadeau: At what age does menopause officially start?
Tes Jordens: The average age for menopause is early 50s. But menopause actually starts the day after you’ve had 12 months of no periods. Menopause is everything after that.
And you can still be in post-menopause at 75. Before that, and including that year of your final periods, is considered perimenopause. And women can be in perimenopause for 10 years.
JN: What are some of the symptoms indicating that a woman is in perimenopause?
TJ: Common things that get talked about a lot is irregularity in your menstrual cycle. But that’s not a requirement. Some women will still cycle regularly but continue to have other symptoms.
Of course, we’ve all heard about hot flashes and night sweats. That’s what most people think about. But there can also be joint pain, fatigue, brain fog, new onset anxiety or worsening anxiety and depression, concentration difficulties.
Honestly, I think the list is growing. [There can be] 50 to 70 different symptoms that a woman can be experiencing.
JN: What I’ve heard from many women is that because a lot of the symptoms can be vague, they are often not addressed by their regular physician. They’re kind of dismissed. Is that what you’ve heard, too?
TJ: Absolutely. That’s part of the reason I’m doing what I’m doing. I’ve been on both sides. I’ve been that provider, and now I’m advocating for those women.
Many medical students and residents were not taught about menopause. It’s not on the radar [of many physicians], so they’re not trained to look for it.
JN: As far as treatment goes, there can’t be one overall thing that you can prescribe or recommend because there’s so many different symptoms. How do you address that?
JT: It all goes back to listening and taking the time to individualize treatment. It depends on each individual woman’s goals, their health risks, what medications they’re currently taking, what treatments they might be undergoing and then their personal preferences.
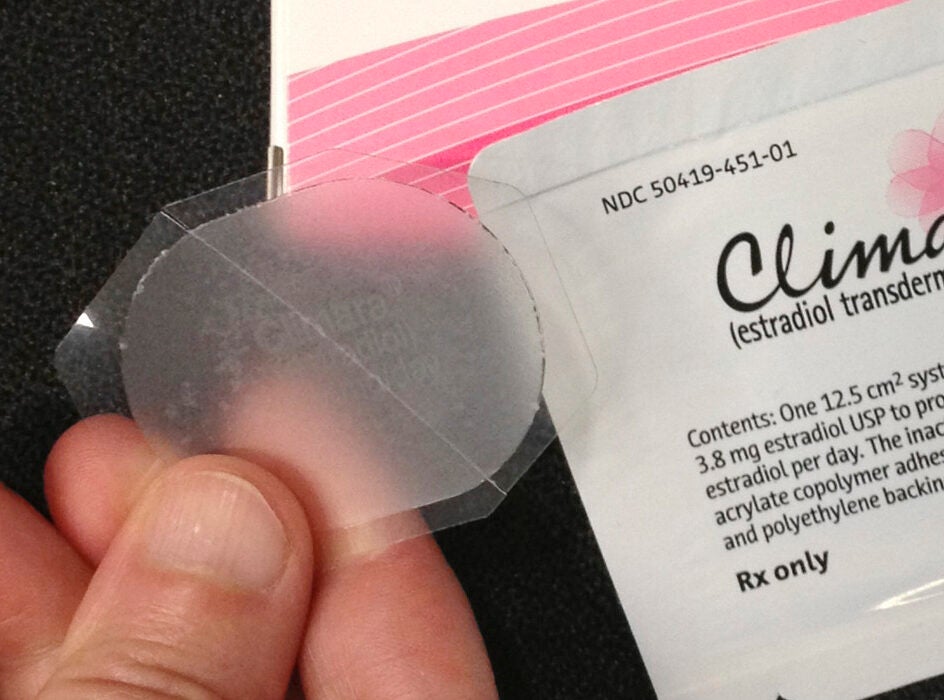
Even though someone may come to see me, it doesn’t necessarily mean that they want medication. They may just want to know how they can mitigate some risks and how to make some good lifestyle choices. Even if you do choose medication — and when I say medication, I’m referring to menopausal hormone therapy — there still isn’t a magic pill or patch. It still [must accompany] lifestyle changes. There are certainly things that women can do to both decrease risk and help themselves feel better.
I would encourage providers — even those who are not going to become menopausal hormone therapy experts — to listen to women, to seek out other providers who are offering this, who are seeking extra education, because we didn’t get it in medical school or nurse practitioner school.

JN: Let’s talk about some of the things you can do to manage menopausal mood swings, hot flashes, chills, the mind fog.
TJ: For mid-life women, one of the big things that I talk a lot about is protein. Protein helps us maintain our glucose, or our blood sugar stability. It also helps us maintain lean body mass as we age. Unfortunately, with declines in hormones like estrogen and testosterone, we just naturally begin to lose lean body mass.
Protein and fiber are besties. They go together. So look at your nutrition. Make sure that you’re eating lots of fruits and vegetables that supports your microbiome. Our microbiome begins to change because of declines in estrogen.
And then movement is important. People should move for movement’s sake. I encourage women to do weight training.
Eliminate screen and device usage two to three hours before bedtime. And if you’re suffering from hot flashes or night sweats, make sure that your bedroom is cool.
And then, of course, menopausal hormone therapy. For lots of women, this is an excellent choice.
JN: What are the options there?
TJ: There are many. Generally speaking, estrogen, progesterone and testosterone are the main actors. Prior to menopause, estrogen supports your menstrual cycle. But we have estrogen receptors from head to our toe. And during perimenopause, estrogen levels go up and down like a roller coaster. That’s when women typically are having the most symptoms. They can get support from Estradiol, a potent estrogen hormone, or another bioidentical. Progesterone can also be calming and aid sleep, so that’s an excellent one, too.
JN: Weight gain usually comes with menopause. Why is that?
TJ: With the decline in estrogen, one of the things that’s changing is our microbiome, and our microbiome helps with a number of things. One of the things is food digestion, which key nutrients we’re latching onto and how we feel in our gut.
The other thing that’s changing is our body’s relationship with insulin and glucose. As estrogen declines, we become less responsive to those. We begin to gain weight, and unfortunately for women, that starts to happen across the midsection. Not only is it something we don’t like, because our pants are tighter, but fat starts to grow around the organs. We call that visceral fat, which increases inflammation, which sets us up for things like diabetes, heart disease and other vascular issues.
JN: Are there any other side effects with these hormone replacement therapies?
TJ: Probably the biggest one is sometimes there will be some bleeding. In perimenopause, that’s probably less troublesome. But in menopause — one of the upsides of which is that you no longer have a menstrual cycle — [bleeding] can be distressing. It can be kind of a nuisance. Typically it happens when you’re just starting or adjusting your dosage of HRT.
JN: What are your thoughts on supplements?
TJ: There are so many supplements out there, and some that have been studied that may be beneficial.
Supplements don’t go through the FDA; they’re not regulated in the same way that medications are. If someone has a particular one [they want to take], I always say I’m happy to look into it to give a patient more educated information.