Hit the gym. Get back in shape.
That’s what many patients with long COVID are told when they talk of the crushing fatigue that envelops them after even a light bout of physical activity.
These symptoms of exhaustion, or post-exertional malaise as it’s called, are a hallmark of long COVID and similar complex illnesses like chronic fatigue syndrome or ME/CFS.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
The idea that exercise can help patients has proven difficult to shake — despite evidence suggesting this isn’t merely a case of deconditioning that patients can overcome by pushing through the pain.
“I don’t think the messaging has been strong enough,” says David Putrino, the director of rehabilitation innovation for Mount Sinai Health System. “It is very clear that this is not a typical response to exercise.”
Now research published this month in Nature Communications gives new weight to this assessment.
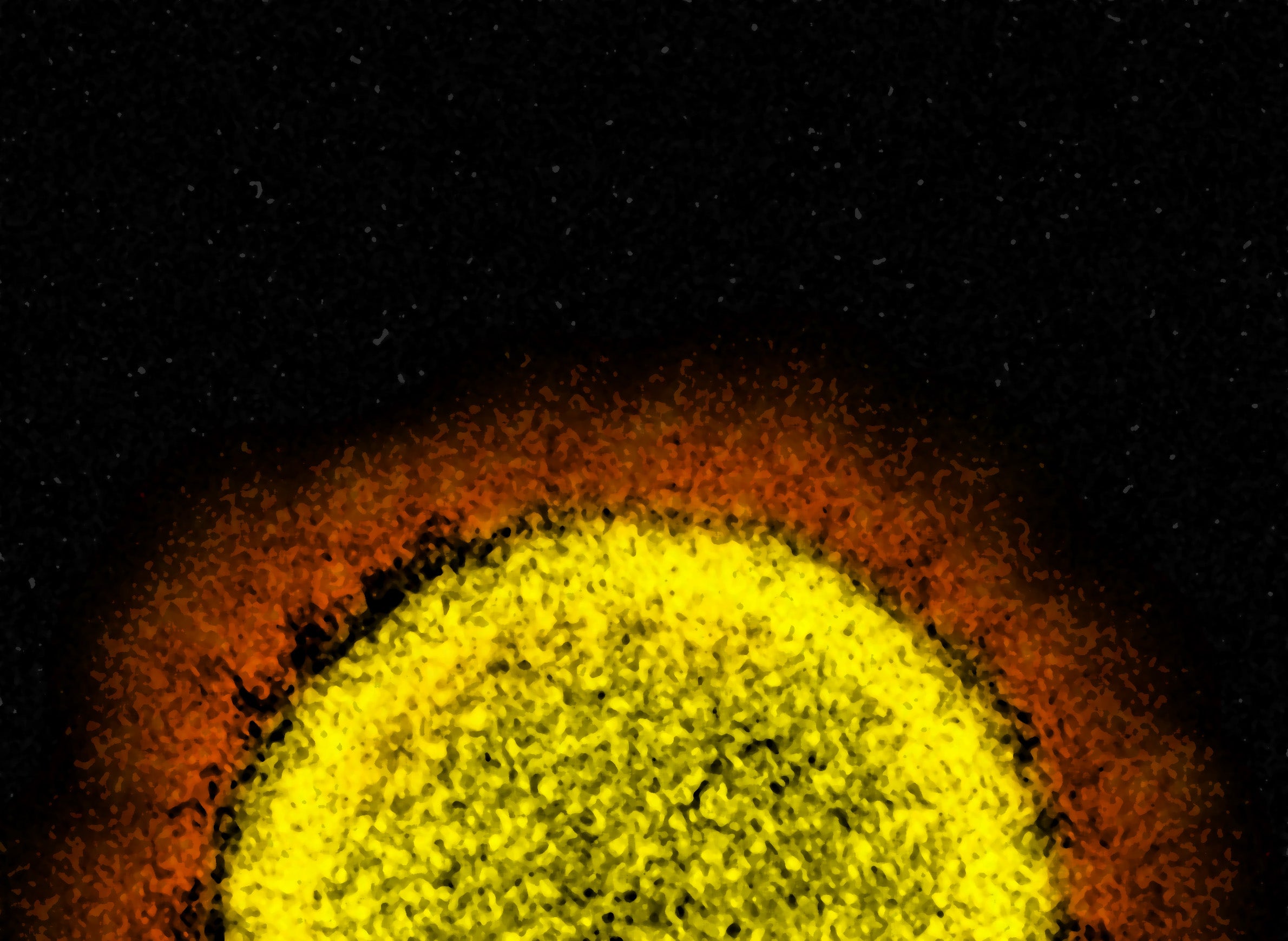
By taking biopsies from long COVID patients before and after exercising, scientists in the Netherlands constructed a startling picture of widespread abnormalities in muscle tissue that may explain this severe reaction to physical activity.
Among the most striking findings were clear signs that the cellular power plants, the mitochondria, are compromised and the tissue starved for energy.
“We saw this immediately and it’s very profound,” says Braeden Charlton, one of the study’s authors at Vrije University in Amsterdam.
The tissue samples from long COVID patients also revealed severe muscle damage, a disturbed immune response, and a buildup of microclots.
“This is a very real disease,” says Charlton. “We see this at basically every parameter that we measure.”
Exercise tests reveal a cellular energy system gone wrong
Most people will get delayed onset muscle soreness after a tough workout, but post-exertional malaise is a different animal altogether.
“It’s not just soreness,” says Charlton. “For a lot of people, it’s completely debilitating for days to weeks.”
While symptoms vary, the most common tend to be muscle pain, an increase in fatigue, and cognitive problems, usually referred to as “brain fog,” that last up to a week after physical exertion.
The study, based at Vrije and Amsterdam UMC health center, compared 25 people with long COVID to healthy controls who’d fully recovered from COVID-19 and had no persistent symptoms. Both groups were asked to work out for about 10-15 minutes on a stationary bike, until gradually reaching their maximum aerobic capacity.
Researchers took multiple blood draws and collected two muscle biopsies from their thighs, a week before they exercised and a day after.
“Their baseline was already impaired and that dropped even lower with the maximal exercise,” says Charlton.
As seen in other long COVID studies, the problem wasn’t related to how their lungs or heart were functioning. Instead, something was making it hard for the muscle to take up the oxygen in the blood.
Using a technique called respirometry, the Dutch researchers oversupplied oxygen to the muscle tissue and found evidence the mitochondria weren’t functioning properly
Further tests revealed more clues
Metabolites in the blood related to energy production were also severely reduced in long COVID patients. And they started producing lactate, a fuel of “last resort” for cells, much sooner during exercise than those who were healthy, yet another sign that their cellular energy system had gone awry.
“The mitochondria are operating at a severely reduced capacity compared to healthy people,” says Charlton.
Taken together, the results support the hypothesis that mitochondrial dysfunction plays a role in long COVID symptoms like fatigue and post-exertional malaise, says Dr. David Systrom, a physician at Harvard Medical School and Brigham and Women’s Hospital.
“They were able to link symptoms to these organic changes,” he says. “I was impressed by that.”
In his own research, Systrom has found evidence of abnormal oxygen uptake by the skeletal muscles during peak exercise in both long COVID and ME/CFS patients, which indicates there’s a problem with oxygen delivery to the mitochondria.
Meanwhile, the Dutch study suggests there could be “intrinsic dysfunction” of the mitochondria’s ability to produce energy, he says.
Systrom says it’s possible both could be happening in long COVID patients. “There may be two ends of that spectrum,” he says. “That’s really something future work will have to look at.”
Biopsies carry clear signs of muscle damage
The story doesn’t end with mitochondria, either.
The muscle biopsies taken after the exercise test revealed other troubling events.
“They end up having a lot more muscle damage than a healthy person would have,” says Charlton. “And because their maximal capacity is now also lower, they have that damage happening at a sooner point.”
A close look at the muscle tissue showed long COVID patients had more atrophy — shrinking of the fibers — than the healthy controls. There were also “immense amounts” of cell death, or “necrosis,” which happens when immune cells infiltrate and degrade the tissue, he says.
The data hints at some kind of altered immune response to exercise in post-exertional malaise.
“It’s not just the functionality of their muscles, but the way that their immune system is receiving that exercise signal,” says Charlton.
The tissue-level analysis of defects in the muscle is “striking” and may help explain the pain, fatigue and weakness that patients experience, says Akiko Iwasaki, a professor of immunobiology at Yale University, who was not involved in the research.
The additional finding that T cells — part of the immune system’s arsenal — had infiltrated the muscles of long COVID patients also caught Iwasaki’s attention,possibly indicating “an autoimmune response within the muscle cells.”
“In the healthy muscle, they find very few, if any T cells,” she says.
Microclots portend big problems for blood vessels
The deep dive into muscle tissue also turned up another increasingly familiar character in long COVID pathology — microclots.
The researchers found these were heavily elevated in those with symptoms — a feature that only got worse following exercise.
Researchers in South Africa have zeroed in on these microclots that carry “trapped inflammatory molecules” as an indication of patients’ compromised vasculature.
In the Dutch study, there wasn’t evidence that microclots were blocking the tiny blood vessels, which was one hypothesis. Instead, they were lodged in the tissue.
The implications of this finding are potentially huge, says Resia Pretorius, a professor of physiological sciences at Stellenbosch University in South Africa, who was not involved in the present study.
“That means the microclots can actually have traveled through the damaged vasculature into the muscle,” she says. “What is scary, but possibly very significant, is that this might be happening in other tissues as well.”
In this scenario, the microclots could reflect the extent of damage to the lining of the blood vessels, which would also impair the delivery of oxygen to the muscle tissue.
If the vasculature is “totally shot,” Pretorius says the “mitochondria will be massively affected,” although more work needs to be done before drawing definitive conclusions.
The underlying causes of long COVID remain elusive; however, one leading theory is that an ongoing chronic infection could be driving the downstream consequences.
The researchers probed this hypothesis. They foundevidence of viral proteins from SARS-CoV-2 in the muscle tissue, but no difference emerged between the long COVID group and the controls, leading them to conclude these are viral leftovers that don’t necessarily figure into post-exertional malaise.
Experts warn that exercise can “harm” and other approaches are needed
The role of exercise in treating post-exertional malaise remains “intensely controversial,” says Harvard’s Systrom, who has studied exercise in the context of other complex chronic illnesses like ME/CFS.
“Post-exertional malaise is a unique symptom in these disorders and is not a feature of deconditioning,” he says. “You cannot simply ask these patients to go to the gym and fix the problem.”
Long COVID is itself an umbrella term that encompasses a wide range of symptoms that may have different underlying causes.
Systrom says it’s possible a subset of these patients may benefit more than others from gradual exercise, especially after successful medical treatment has been first established.
In their study, Charlton says they looked at other research to verify that what they observed did not stem from physical inactivity. He also notes that the long COVID patients who were enrolled were not bedridden and had an average of 4,000 steps a day.
Putrino at Mount Sinai considers the study a much-needed wake-up call for the broader medical field — clear evidence of a biological basis for the energy crash and onslaught of symptoms that patients with long COVID and similar conditions experience.
“As opposed to what’s been sold to patients over the last few decades, that symptoms such as extreme fatigue and exertional malaise are psychological or physical conditioning issues,” he says. “Physical exertion does harm to the bodies of people with these illnesses.“
His general guidance is to avoid exercise if you have post-exertional malaise and instead practice “energy conservation.”
At his clinic, Putrino prescribes what’s called “autonomic rehabilitation” for these patients.
Whereas the aim of exercise is to improve cardiovascular fitness — something he might recommend to patients who’re recovering after severe pneumonia — this type of rehabilitation is done at a much lower intensity and duration, and it takes into account post-exertional malaise.
“We need to step out of this erroneous mindset of no pain, no gain,” he says.
9(MDAyMjQ1NTA4MDEyMjU5MTk3OTdlZmMzMQ004))
© Copyright 2026 by NPR. To see more, visit https://www.npr.org.9(MDAyMjQ1NTA4MDEyMjU5MTk3OTdlZmMzMQ004))