Hannah Miller, a nursing student and employee of a long-term care facility in Eau Claire, Wisconsin, received her first dose of the COVID-19 vaccine Aug. 23 — and not voluntarily.
“(The vaccine) hasn’t been out long enough to know what long-term effects are,” Miller told Wisconsin Watch. “We don’t know if it could cause bigger health issues in the future or cause issues, such as fertility.”
Miller said she was required to receive the vaccine by the hospital where she is completing her clinicals for school. She said she would not be able to graduate without getting it. Miller asked that her school and her workplace not be disclosed in this article.
News with a little more humanity
WPR’s “Wisconsin Today” newsletter keeps you connected to the state you love without feeling overwhelmed. No paywall. No agenda. No corporate filter.
Increasingly, health care facilities in Wisconsin and around the country require their employees to be vaccinated. Yet in long-term care facilities such as nursing homes — where residents are highly susceptible to severe illness and death from COVID-19 — some workers refuse the shot.
As of late August, Wisconsin’s rate of fully vaccinated nursing home employees was around 60 percent. Wisconsin’s total rate of fully vaccinated individuals between the ages of 18 and 64 is about 58.4 percent. By contrast, the rate among residents 65 and older is around 95 percent.

In mid-August, President Joe Biden ordered long-term facilities that receive federal Medicare or Medicaid funding to require their workers to be vaccinated, citing studies that show having a highly vaccinated nursing home staff is associated with a 30 percent reduction in COVID-19 cases. Of the 355 nursing homes in Wisconsin, 353 are Medicare and Medicaid certified. Still, some Wisconsin nursing homes are not requiring staff to be vaccinated, a spot check of facilities by Wisconsin Watch showed.
Nationwide, more than 134,000 long-term care facility residents have died from COVID-19. In Wisconsin, 3,220 people have died in such facilities as of Sept. 3 — or 42 percent of all COVID-19 deaths in the state, the Wisconsin Department of Health Services reports. In one of the worst outbreaks in Wisconsin, DHS found 191 residents and workers were infected in a single unnamed nursing home.
The president’s decision to issue the mandate was prompted by a Centers for Disease Control and Prevention study which found the effectiveness of the Pfizer and Moderna vaccines is waning among nursing home residents — among the first to be vaccinated in early 2021.
Decreasing vaccine-induced immunity and the emergence of the highly infectious delta variant may be to blame, the researchers said.
“Because nursing home residents might remain at some risk for … infection despite vaccination, multiple COVID-19 prevention strategies, including infection control, testing, and vaccination of nursing home staff members, residents, and visitors, are critical,” the study recommended.

FDA OK Doesn’t Erase Unease
As a health care employee, Miller said she will continue to do her part to keep the people around her safe by wearing a mask and washing her hands. However, Miller pointed out that the vaccines “didn’t eradicate the disease,” and she could still catch it even if she’s vaccinated.
She believes it’s too soon for a mandate. Miller said she has family members who work in health care who have quit their jobs instead of getting a required shot.
The CDC finds in a new report that unvaccinated people are 29 times more likely to end up hospitalized with COVID-19 than vaccinated people. As for Miller’s concern about her ability to have children, the CDC advises that “currently no evidence shows that any vaccines, including COVID-19 vaccines, cause fertility problems (problems trying to get pregnant) in women or men.”
“I fully encourage vaccines once they have been tested and are FDA approved,” Miller said. “Vaccines are valuable and are needed, but I don’t want to be the guinea pig. I still believe everyone should have their freedom on whether to be vaccinated or not.”
Days after Miller spoke with Wisconsin Watch, the Pfizer vaccine was granted full approval by the Food and Drug Association. Still, she hesitated to endorse it.
“I feel better now that they have approved it, but I’m still nervous about what could possibly still happen in the future,” Miller said of the change. “It usually takes years for the FDA to approve a vaccine and this one was done so fast that I feel it may have been rushed to convince more people to get it and I feel like there is still information missing.”
Strife Over Vaccine Mandates Continues

The Wisconsin Health Care Association and the Wisconsin Center for Assisted Living are promoting vaccination among long-term care staff. But their national organizations warn vaccine mandates could worsen a shortage of workers in the industry. Graphic courtesy of https://www.whcawical.org/getvaccinated/
Miller isn’t the only long-term care facility employee concerned about vaccine mandates. In recent weeks, health care workers have protested at the state Capitol and outside their places of work.
And the nation’s leading nursing home association worries the existing severe labor shortage in long-term care will only grow with a vaccine mandate. In Wisconsin, nearly 1 out of every 4 jobs remains unfilled, according to the Wisconsin Health Care Association and Wisconsin Center for Assisted Living.
Rock County’s Rock Haven nursing home in Janesville is one example of a facility that tried to implement such a policy. In December, the county-run nursing home mandated staff vaccinations, prompting legal action from some employees. They claimed the rule was a violation of their rights to “decide whether to accept or refuse administration of the COVID-19 vaccines.” In response to the legal challenge, the Rock County Board rescinded the mandate in late May.
Marilyn Burns, Rock Haven’s infection preventionist, released a statement confirming there is no vaccine mandate at the nursing home — which is currently battling a COVID-19 outbreak.
“We understand some members of the Rock Haven community are unhappy with Rock Haven employing unvaccinated staff,” the statement said, adding, “We are unsure how this (Biden) mandate will affect our facility.”
Wisconsin Vaccination Rate 32nd
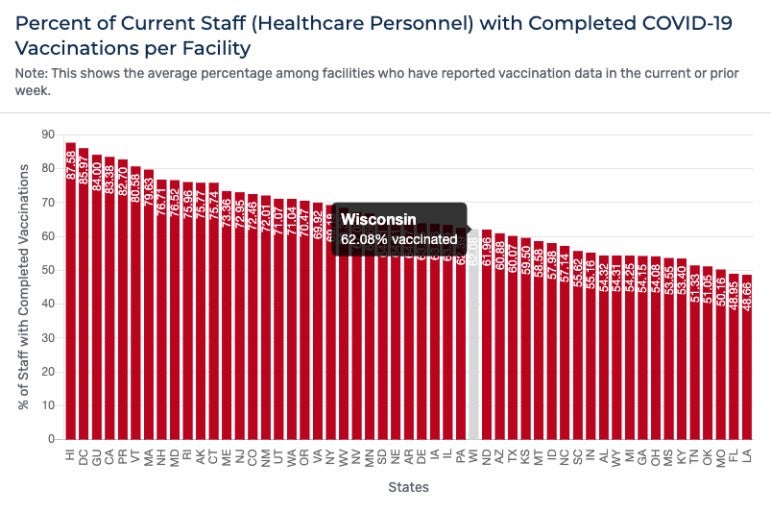
In late August, Wisconsin’s rate of fully vaccinated nursing home employees was around 62 percent. The state is ranked 32nd among the 50 states, Puerto Rico, Guam and the District of Columbia.
Hawaii leads the country with a long-term care facility staff vaccination rate of around 88 percent. Louisiana was last at 49 percent.
DHS said vaccines are the “most important tool” to protect people from COVID-19 and that “it is vitally important” that employees of long-term care facilities get vaccinated.
As of Sept. 5, the agency had conducted 2,678 public health investigations related to COVID-19 at long-term care facilities around Wisconsin. It found the median number of confirmed cases per investigation is three, the average is 11, with one unnamed facility reporting 191 confirmed cases of COVID-19.
In Wisconsin, an investigation of a long-term care facility is automatically launched whenever a case of COVID-19 is detected, including an examination of how the person may have gotten infected, said Elizabeth Goodsitt, DHS communications specialist.
Although the total number of active investigations has declined over the past year, DHS has reported a steady uptick over the course of the summer.

Labor Shortages Feared
Also rising are concerns in the long-term care industry around Biden’s vaccine mandate. In a statement, Mark Parkinson, president and CEO of the American Health Care Association and National Center for Assisted Living, objected to Biden singling out one health care provider group.
“Focusing only on nursing homes will cause vaccine hesitant workers to flee to other health care providers and leave many centers without adequate staff to care for residents,” the statement said. “It will make an already difficult workforce shortage even worse. The net effect of this action will be the opposite of its intent and will affect the ability to provide quality care to our residents.”
After Parkinson spoke to Wisconsin Watch, the Biden administration announced a series of steps to help curb the surging pandemic — an expansion of his earlier efforts to vaccinate federal employees. On Thursday, Biden said a federal rule will require all businesses with 100 or more employees to mandate each employee be vaccinated against COVID-19 or submit to weekly testing. Biden also said he plans to extend a vaccination requirement for workers at long-term facilities receiving federal Medicare or Medicaid funding to all medical facilities, including hospitals and at-home care.
The emergency rule is for private sector employers and would apply to some 80 million workers. The “six-pronged” plan will impact about 100 million people.
Ultimately, Miller said she believes all people — including health care workers — should be allowed to control their own health care, not the government.
“In nursing school we are constantly taught that the patient has rights,” Miller told Wisconsin Watch. “They can choose to not take medications, decline treatment or refuse exams. We are patients in our own way, so why don’t we have those same rights to refuse?”
Madeline Fuerstenberg’s work on this story was sponsored by the Ann Devroy Fellowship at the University of Wisconsin-Eau Claire. The nonprofit Wisconsin Watch (wisconsinwatch.org) collaborates with Wisconsin Public Radio, PBS Wisconsin, other news media and the University of Wisconsin-Madison School of Journalism and Mass Communication. All works created, published, posted or disseminated by Wisconsin Watch do not necessarily reflect the views or opinions of UW-Madison or any of its affiliates.





