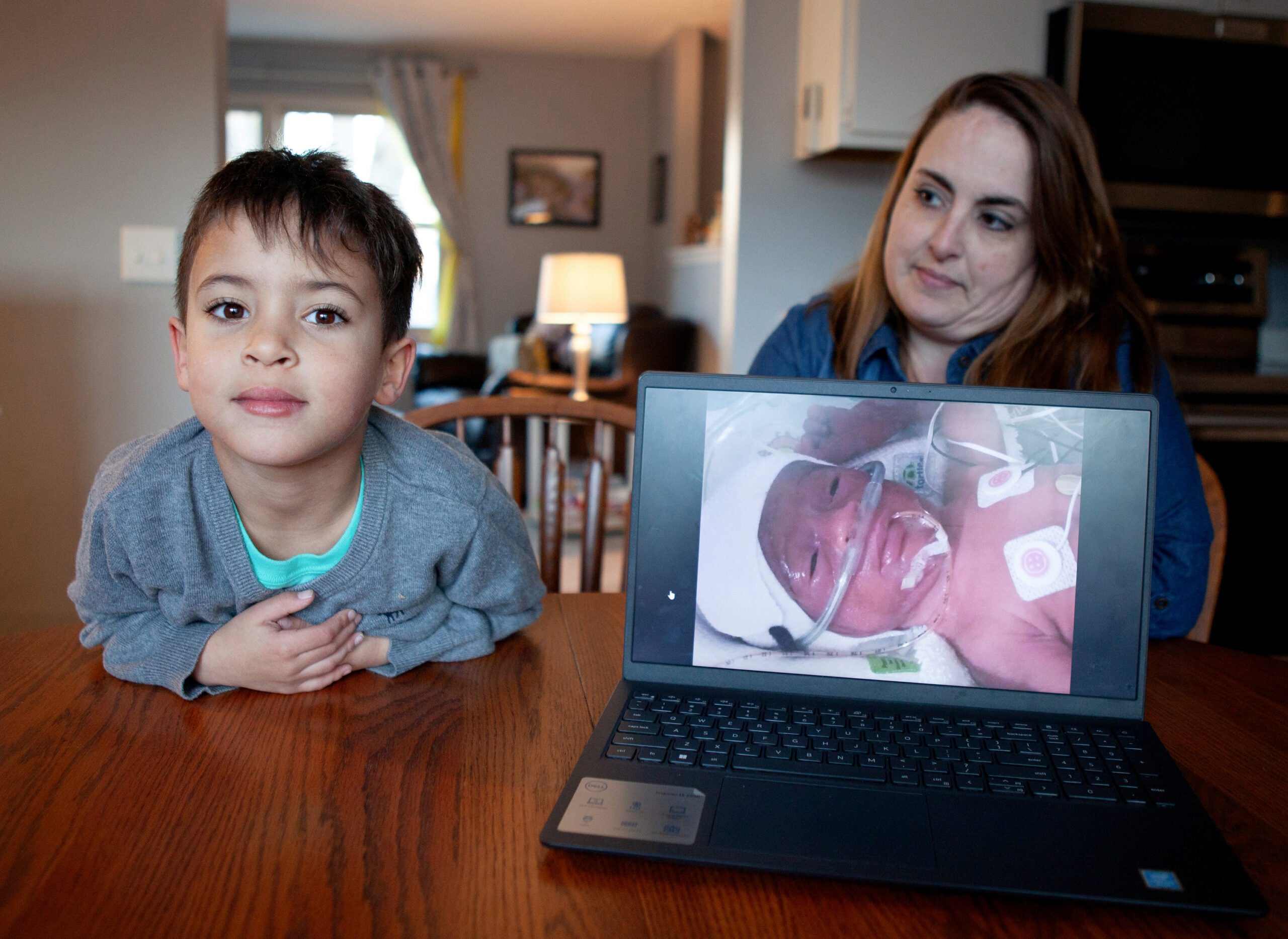
As the situation surrounding COVID-19 rapidly changes, there is increasing concern about at-risk populations. Evidence from the COVID-19 outbreak shows some populations, like the elderly, are more vulnerable to the virus.
Many are wondering if pregnant women are also at a higher risk.
WHYsconsin has received numerous questions from audience members about COVID-19 and we are working to answer them. WPR’s Mary Kate McCoy spoke with Dr. Ken Merkitch, an OB-GYN with Gundersen Health System, to answer some of the questions raised about COVID-19 and pregnancy.
Stay informed on the latest news
Sign up for WPR’s email newsletter.
The interview has been edited for brevity and clarity.
Q: Are pregnant women at a higher risk of contracting COVID-19?
Ken Merkitch: There’s not a ton of data on this. The best article that looked at the experience was from The Lancet with nine women in pregnancy in China. They all developed it in the third trimester, so late in the pregnancy. China has a really high caesarean section rate, and they all had caesarean sections. But they didn’t seem to find any specific problems with those babies whose mothers had COVID-19.
It’s thought right now that it’s not transmitted intrauterine, that is if a woman has an infection, that it doesn’t become a viremia (presence of virus in the blood) that will cross the placenta.
Now, the only thing that argues a little bit against that is that there has been a report that two people in London delivered, and I believe both by C-section, who had COVID-19 and their babies were culture positive for COVID-19 soon after delivery.
But to my understanding at this point in time, none of those children have had bad outcomes. We know COVID-19 is transmitted through contact, obviously if you’re having a C-section you’re contacting skin.
A concern has been, would pregnancy be a higher risk for women if they develop COVID-19? At least from the very, very small amount of data from the Chinese experience, that answer seems to be no, but we’re still at the very outset of our knowledge in this regard.
Q: How can pregnant women protect themselves?
KM: Just like we’re recommending to everybody. At Gundersen, we are calling patients in advance to come in because you have a baby who is maybe growth restricted or you have diabetes or hypertension, and we need to monitor you very closely for these things.
Traditionally we see people every four weeks in pregnancy until the latter parts of pregnancy. If you have a problem, we want you to call us so that we’ll see you. But if you’re doing well and your baby’s moving well and you’re low risk, we don’t have to see you until your next visit.
We don’t have an effective antiviral agent. We certainly don’t have a vaccine. The best thing we can do at this point is social distance. Any chance we have to keep people at home and not interacting with other people who could be vectors is probably the best thing we can do right now.
Q: What effect does COVID-19 have on unborn children?
KM: To the best of our knowledge, nothing at this point. Again, mostly because this virus would seem to be a respiratory virus that doesn’t really cause viremia. It stays in the respiratory tract as far as we know. It does kill people, but the good thing about it is it doesn’t seem to transmit to other organs, including to the best of our knowledge at this point, the placenta.
Q: What about after delivery?
KM: If you have COVID-19 and you deliver, the current recommendations from the Centers for Disease Control and Prevention is that you should separate from your baby until your quarantine is over, which is obviously a very difficult thing for new mothers to have to do. And frankly, even the CDC admits this.
There will come a point where, you know, where will we put these babies? We’re going to run out of hospital rooms. The fallback is that you should separate from your baby by a curtain to try to prevent droplet transmission.
If you choose to breastfeed, and certainly breastfeeding is the best thing we can do for our newborns — (we ask) that you practice careful hand-washing, wear a mask.
For breastfeeding, there is some preliminary data that when the mother has COVID-19, they’re starting to develop antibodies. And so those antibodies can be transmitted through breast milk, or may be transmitted through the breast milk, and may be helpful. So this is an area that is evolving.
Q: If the situation continues to worsen and hospitals fill up with COVID-19 patients, will it be safe to give birth in the hospital?
KM: The American College of Obstetricians and Gynecologists have published significant data on this. And if you deliver at home, you are three times more likely to have your baby die than delivery at a hospital. Most women who deliver at home are low risk, so that’s comparing low risk women to women of variable risks.
It is still safest to deliver in a hospital because so many things can happen that can go wrong so quickly.
Wisconsin Public Radio, © Copyright 2024, Board of Regents of the University of Wisconsin System and Wisconsin Educational Communications Board.